I’m an Oncologist – Why We Think Oral Sex Is Fueling the Rise in Throat Cancer
Oncologists are increasingly looking to oral sex as the leading cause of a steady increase in throat cancer rates.
The number of cases of this disease has been rising slowly but consistently since the mid-2000s, by about one percent per year.
And while it is more common in older adults, oropharyngeal cancer is increasingly diagnosed in young people due to increased rates of human papillomavirus.
Dr. Hisham Mehanna, an oncologist at Britain’s University of Birmingham, wrote in the Conversation that the number of sexual partners over a lifetime, especially oral sex, is the most important risk factor for this specific type of throat cancer.
People who have oral sex with at least one in six people with HPV during their lifetime are 8.5 times more likely to develop cancer of the throat, cervix or genitals compared to those who do not practice oral sex.
This graph shows how the number of new cases of throat cancer in the US has increased since 1999. It increases by about one percent per year in women and three percent in men.
Research shows that more than 80 percent of men and women practice oral sex, and surveys show this is the case especially among womenfrom 85 percent reporting oral sex between 2011 and 2013, to 89 percent between 2017 and 2019.
A majority of throat cancers – about 70 percent – are caused by human papillomavirus (HPV), an umbrella of common sexually transmitted viruses that generally cause no symptoms and go away on their own.
There is a highly effective vaccine against HPV, but the numbers are significantly lower than the 85 percent needed to achieve “herd immunity,” the term meaning enough people have been made immune so that the virus cannot spread.
Fewer than 60 percent of schoolchildren have received the HPV vaccine for a variety of reasons, including parental hesitancy and anti-vax sentiment.
HPV strain 16 is strongly linked to mouth and throat cancer. In recent years, the incidence of these HPV-related cancers has risen significantly, largely due to shifts in sexual behavior, including the increased practice of oral sex. Henry Ford Health.
Dr. Mehanna called on parents around the world to get their children vaccinated as the vaccinations are highly effective.
He said the vaccines only work if coverage among girls is high — more than 85 percent, “and only if one stays within the covered ‘herd.’
‘It certainly does not provide protection in countries where vaccination rates for girls are low, for example the US, where only 54.3 percent of adolescents aged 13 to 15 had received two or three HPV vaccination doses in 2020.’
He added that the coronavirus pandemic has created additional challenges.
First, schools were inaccessible for a time, making it more difficult to reach young people. Additionally, increasing vaccine hesitancy or “anti-vax” sentiment in several countries may contribute to lower vaccination rates.
At the same time, condom use among young people is at a record low.
To map out what condom use entails in relation to gender, age, race and education level, an independent sample was conducted from 2011 to 2015 among men and women between 15 and 44 years old.
When participants were asked about their last sexual experience, only 33.7 percent of men and 23.8 percent of women used a condom.
The survey was the first to examine Americans’ struggles with condoms during sex, from some who said it “fell off completely” to others who only used it for part of the act.
More than 58,000 Americans was diagnosed with mouth or throat cancer in 2024.

Those with six or more lifetime oral sex partners are 8.5 times more likely to develop oropharyngeal cancer than those who do not practice oral sex
While 69 percent of diagnosed people survive longer than five years after diagnosis, the US recorded 12,230 deaths this year.
Meanwhile, about one in four Americans has HPV, although most don’t know it due to a lack of symptoms. This can be dangerous because more than 11,000 women with HPV develop cervical cancer.
If someone who receives oral sex has HPV, he or she can pass it on to the person performing the sex.
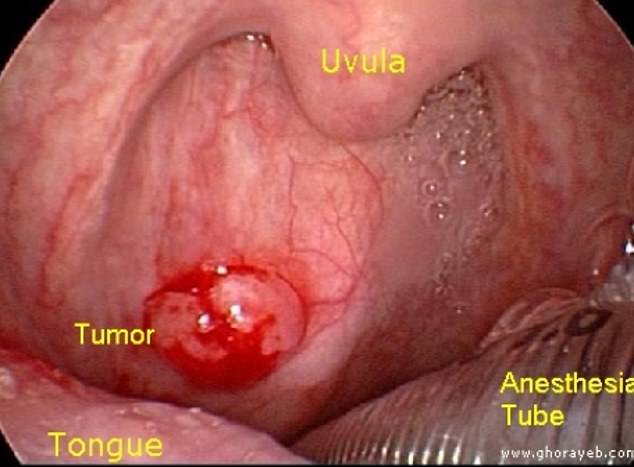
When the virus enters the body through the throat, it settles in deep crevices.
It disrupts the cell life cycle and cell death in the throat wall, causing some cells to grow uncontrollably.
This can lead to the formation of cancer cells that continue to accumulate until they cause a tumor.
It usually takes years for the virus to develop into throat cancer.
HPV causes oropharyngeal cancers in approximately 60 percent. Photo courtesy of medbullets.com
About 10 percent of men have oral HPV and 3.6 percent of women, usually at an older age.
Most people with HPV will not develop any symptoms, and the immune system usually clears them up within a few years. But people with some kind of defect in their immunity are more likely to develop genital warts or mouth warts or cancer of the cervix and genitals.
In 2006, a vaccine against HPV was introduced for children aged 11 and older, although initially for girls. It was approved for boys in 2020.
Although some side effects have been reported, including fever, fatigue and headache, 96 percent of these effects were considered non-serious, and the benefits of the injection have been proven to far outweigh the risks.
The HPV vaccination rate is relatively low, around 60 percent of teenage girls, compared to other developed countries such as Britain, where 85 percent of teenage girls have been vaccinated.
Unlike the U.S., the British government offers a universal HPV vaccination program that is free for eighth-grade students, bringing the country closer to eradicating cervical cancer.
Getting vaccinated as a teen is just as crucial for preventing oropharyngeal cancer, as HPV has been shown to cause 60 to 70 percent of cases.
