HIV cases among African-born Brits outnumber those from UK for first time in a decade
More HIV cases were diagnosed among people born in Africa than in Britain last year, according to official figures.
Data from the UK Health Security Agency shows that 3,805 people were diagnosed with human immunodeficiency virus (HIV) in England in 2022.
About 700 were born in Britain, a record low. Meanwhile, 1,179 have been born in Africa – the highest number since 2014.
It reverses a decade-long trend in which the highest number of HIV cases are detected among people born in Britain.
The UKHSA data shows that the number of HIV diagnoses has increased by 22 percent – from 3,118 in 2021 to 3,805 in 2022.
The UKHSA data shows that despite the number of HIV diagnoses increasing by 22 per cent – from 3,118 in 2021 to 3,805 in 2022 – the number of detected HIV diagnoses among those born in Britain has fallen to a record low of 700.
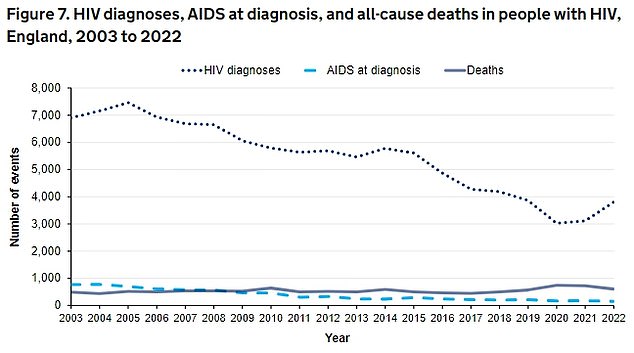
UKHSA data shows the number of HIV diagnoses has increased by 22 per cent – from 3,118 in 2021 to 3,805 in 2022
It means that, proportionately, 18 percent of HIV cases were among those born in Britain.
Three in ten cases were among those born in Africa (31 percent), while about a tenth were seen among people born in Europe (10 percent) and Asia (9 percent).
The place of birth was unknown in a quarter of the cases.
The remaining cases came from Latin America and the Caribbean (6 percent), North America (0.7 percent) and Oceania (0.2 percent).
Most of the increase in HIV diagnoses is ‘attributable to people previously diagnosed abroad’, which is likely to have been acquired abroad and ‘does not reflect an increase in transmission in England the UKHSA said.
It noted that 1.1 million people were tested for HIV in 2022 – a 10 percent increase from 2021. It includes almost 200,000 tests among gay, bisexual and other men who have sex with men – the highest number ever recorded.
However, the overall testing rate remains 15 percent lower than pre-pandemic levels.
Half of all tests belonged to those who ordered them online.
In total, there were 94,397 people diagnosed with HIV in England, half of whom were aged 50 or over. Nearly all (98 percent) were virally suppressed – meaning they could not pass the virus on to sexual partners.
HIV damages the cells in the immune system and weakens the body’s ability to fight everyday infections and diseases.
The virus is spread through the bodily fluids – such as semen, vaginal and anal fluids, blood and breast milk – of an infected person. However, it cannot be spread through sweat, saliva or urine.
It is usually transmitted through condomless anal or vaginal sex.
Tests are the only way to detect HIV. They are available from GPs, sexual health clinics, some charities and online and involve taking a sample of saliva or blood.
A preventive HIV medicine, pre-exposure prophylaxis (PrEP), can also be prescribed to people over 16. It reduces the risk of HIV infection when taken properly.
Those who take post-exposure prophylaxis (PEP) – an anti-HIV drug – within 72 hours of exposure can prevent becoming infected in the first place.
For those who are infected, there is no cure for HIV.
But antiretroviral therapy (ART) – which stops the virus from replicating in the body, allowing the immune system to repair itself – allows most to live healthy lives.
Levels of the virus in those on ART will drop so low that they can have condomless sex without passing HIV to their partner – although this can take up to six months.
AIDS (acquired immunodeficiency syndrome) is the name used to describe a range of potentially life-threatening infections and diseases that occur when your immune system is severely damaged by HIV.
However, those who are diagnosed with HIV early and begin treatment will not develop AIDS-related diseases and will live a near-normal lifespan.
