Doctors DON’T always know best, experts say as they urge GPs to ditch ‘paternalistic’ view and take patients more seriously
Doctors have been urged to ditch the age-old 'doctor knows best' attitude when diagnosing diseases.
Experts said the “paternalistic and often dangerous” view should change “towards a more equal relationship” that takes into account patients' own experiences.
It comes as a study led by the University of Cambridge and Kings' College London found that a patient's views on their own symptoms or illness are not valued by the majority of doctors.
Patients described how they felt 'degraded and dehumanized'.
Researchers analyzed data from 676 patients and 400 physicians were surveyed about their experiences diagnosing neuropsychiatric lupus (NPSLE), an incurable disease that is notoriously difficult to diagnose.
GP workforce data for May 2023 shows there are 27,200 fully qualified GPs in England. This is a decrease compared to the 27,627 a year earlier. The GP number peaked in March 2016 at 29,537
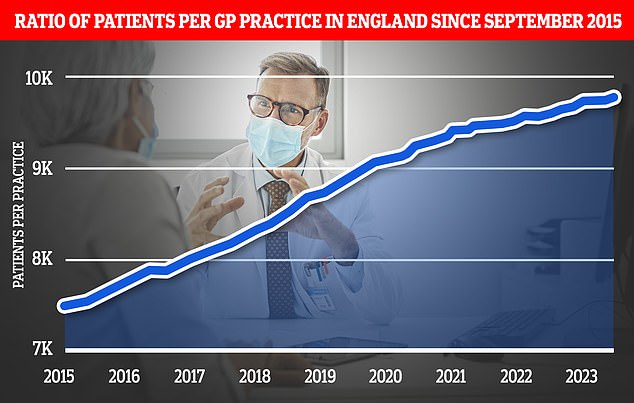
Chart shows the ratio of GP patients to practices since 2015, with an average of 9,755 patients per surgery in May 2023
The condition has 'invisible symptoms' such as headaches, hallucinations and depression, with no specific biological test, meaning diagnoses are often based on the patient's reported symptoms.
Despite this, the study revealed that doctors viewed patients' self-assessments as the least important of the thirteen different types of evidence used in diagnoses. These also include brain scans and response time to treatment.
Patient self-assessments were ranked among the top three most important by only 3.8 percent of all physicians surveyed.
Doctors considered their own assessments to be the most important factor, even though they could not trust 'invisible' symptoms.
Nearly half (46 percent) of all patients surveyed said they had never or rarely been asked for their self-assessment of their disease, according to the research funded by the Lupus Trust and Lupus UK.
Just under a quarter (24 percent) also reported that their self-assessment of disease activity was never or rarely consistent with that of their doctors.
Writing in the diary RheumatologyResearchers said male doctors were more likely to believe patients were exaggerating their symptoms.
Ethnicity and gender were also thought to influence diagnosis, particularly the perception that women were more likely to be told their symptoms were psychosomatic.
An anonymous patient shared his diagnosis experience with the research team, saying: 'You give up control of your own body, and I will tell them my symptoms and they will tell me that the symptom is wrong or I can't feel it anymore . pain there, or that way.”
They added: 'The whole thing has taken so long, and is humiliating and dehumanizing… If I had put the expertise of doctors above my own, I would be dead.'
A GP in England also told researchers: 'It is common for women in particular to be told that their symptoms are psychosomatic… once emotion is shown, all too often it becomes the cause of everything else. This bias causes medical negligence.”
Sue Farrington, co-chair of the Rare Autoimmune Rheumatic Disease Alliance, said: 'It is time to move from the paternalistic and often dangerous 'doctor knows best' to a more equal relationship where patients with lived experiences and doctors with learned experiences work more together.'
Meanwhile, Dr Melanie Sloan, lead author of the study and a public health and primary care researcher at the University of Cambridge, added: 'It is incredibly important that we listen to patients' insights and their own interpretations of their symptoms and appreciate these, especially those with long-term complaints. diseases.
'After all, they are the people who know what it is like to live with their condition.'

NPSLE affects the brain, spinal cord, or other nerves, causing symptoms such as seizures, strokes, and psychosis. Despite this, the study found that doctors considered patients' self-assessments to be the least important of the 13 different types of evidence used in diagnoses. These also include brain scans and response time to treatment
However, the researchers acknowledged that some doctors valued patients' opinions. Others also raised concerns about the effectiveness of diagnostic test evidence.
A psychiatrist interviewed for the study told the team: 'Patients often come to the clinic having had multiple examinations, examining their own condition at a very high level and working hard to understand what is going on with their own body is… they are often experts. diagnosticians in their own right.'
Another neurologist added: 'The disease affects your blood vessels, we often can't test for this, but that's very systemic, the nerves in your blood vessels are everywhere, so why wouldn't that explain a lot of these neurological problems? symptoms that these lupus and other autoimmune patients get?
“There is a systemic diffuse presentation that is very difficult to pinpoint when physicians think in that very limited framework of neurology.”
Senior study author Dr Tom Pollak, from the Institute of Psychiatry, Psychology and Neuroscience at King's College London, added: 'No human being will always be able to accurately pinpoint the cause of symptoms, and both patients and doctors can do this be wrong. .
'But combining and appreciating both views, especially when diagnostic tests are not advanced enough to always detect these diseases, can reduce the number of misdiagnoses and improve relationships between doctors and patients, which in turn leads to greater trust and more openness in reporting symptoms.”
