Woman, 22, dies from cannabis-induced vomiting that triggered fatal heart disorder before doctors declared her brain dead
A chronic marijuana user died after a severe, multi-day bout of vomiting and abdominal pain caused a fatal cardiac arrhythmia that led to brain death.
The 22-year-old woman treated in Canada started using cannabis at the age of 14 and had suffered from multiple bouts of severe cannabis hyperemesis syndrome – a condition characterized by violent, painful, repeated episodes of severe vomiting – for more than three years.
When she was admitted to the hospital with vomiting and abdominal pain, she developed a specific life-threatening irregular heartbeat called torsades de pointes, which caused her heart to stop.
While doctors were able to restart her heart, her brain had already suffered a catastrophic loss of oxygen and she was declared brain dead four days later.
Cannabis hyperemesis syndrome can develop with regular marijuana because the drug can cause certain receptors in the brain to malfunction.
In people new to cannabis use or those who do not use it regularly, signals to the cannabinoid receptors in the brain and gastrointestinal tract usually continue to function normally.
But with chronic marijuana use, those receptors become desensitized and don’t respond to the drug in the same way, disrupting the body’s natural ability to control nausea, which can lead to cannabis hyperemesis syndrome.
CT scans of the woman’s brain showed the extent of the damage caused by a lack of oxygen when her severe vomiting caused a fatal irregular heartbeat. The brain folds are flattened and the entire brain is swollen
The woman’s cause of death was ultimately attributed to a fatal irregular heartbeat, exacerbated by low potassium levels caused by her frequent vomiting and by medications that can affect the heart rhythm.
She also had genetic mutations that contributed to her heart problems and was taking haloperidol and ondansetron, an antipsychotic and an anti-nausea drug, respectively.
According to the Toronto doctors who wrote the case report published in the journal Springerlinkonly two other deaths from cannabis hyperemesis syndrome have been described in the medical literature.
In the six months prior to the woman’s hospitalization, she visited the emergency department six different times with episodes of vomiting and nausea that lasted about a week each time.
She had low potassium during almost all of her emergency department visits. To treat this she was given fluids and electrolytes.
Low potassium levels can lead to muscle cramps and weakness, heart rhythm disorders, kidney stones and digestive problems.
During her severe episodes, and to prevent them at home, she was treated with a combination of medications, including various anti-nausea, anti-anxiety, and sedative medications.
On the day of her hospitalization, the woman arrived at the ER around 9:30 a.m. and was found to have a low heart rate and high blood pressure. Her potassium was also low, indicating an electrolyte imbalance.
During the afternoon, she was given potassium through an IV, as well as several other medications, until about 6 p.m. The last medication she received was the anti-emetic dimenhydrinate.
But 25 minutes later, nurses checked her and found no vital signs. As doctors tried to revive her, they used an electrocardiogram (ECG) to monitor her heart rhythm.
Initially, the ECG detected ventricular fibrillation, a serious condition in which the lower chambers of the heart lose their ability to pump normally, causing the heart rhythm to become chaotic and disorganized.
After being shocked with a defibrillator in an attempt to restart her heart, her rhythm deteriorated to the point where the heart rate showed a twisting pattern on the ECG known as torsades de pointes, a fatal form of arrhythmia: a irregular heartbeat.
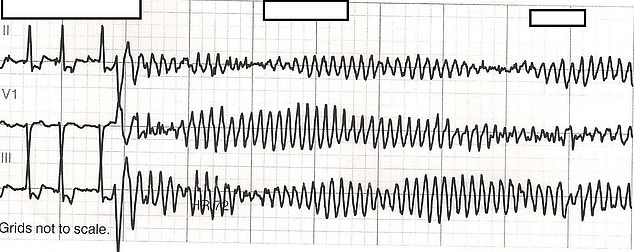
The woman’s heart rate was disorganized and at times very low and at other times very high. The photo above is an example of an irregular heat stroke
Doctors restarted her heart, but her brain’s ‘downtime’ had been longer than 30 minutes, meaning it had been deprived of crucial oxygen, killing brain cells that left her in a vegetative state.
She was declared brain dead, taken off life support four days later and died.
Cannabis hyperemesis can potentially be caused by any form of cannabis, from smoking and vaping to edibles, although the case study does not say how the woman consumed her cannabis.
The condition causes compulsive vomiting that is often painful and includes forceful gagging. Long-term use of cannabis causes a buildup of cannabinoids and other toxins in the body, affecting receptors in the brain and gastrointestinal tract, leading to nausea and vomiting.
It can also affect the motility and function of the gastrointestinal tract.
A unique sign of CHS is the temporary relief you get when you take a hot shower, and people with the condition often take several showers a day to reduce nausea.
CT scans of the woman after her death, which examined the extent of her brain damage, showed that the grooves in her brain had been flattened, her entire brain had swollen and the boundary between the outer layer of the brain and the inner layer was not properly defined. , indicating widespread damage caused by a lack of oxygen.
Cannabis use has seen a rapid increase over the past decade, culminating in legal recreational use in 24 states.
And while it has been shown to have benefits for epilepsy and chemotherapy-related nausea, daily use of the drug has also proven to be extremely risky.
Cannabis use disorder is loosely defined as people who smoke marijuana every day and cannot stop using the drug, even though it causes health and social problems, such as affecting their work and relationships.
It affects about 30 percent of users, although that may be underestimated.
A study by Canadian researchers last year compared people who had been diagnosed with cannabis use disorder with those who had not.
During the study period, 721 (2.4 percent) of people in the cannabis use disorder group experienced their first cardiovascular event, such as a heart attack or stroke, compared to 458 (1.5 percent) of people in the group that did. do not abuse the drug.
Adults with a cannabis use disorder had an approximately 60 percent higher risk of heart attacks and strokes than those without the disorder.
Cannabis can also harm a person’s sleep health. Daily marijuana users were more likely to have insomnia than non- and even occasional users.
According to a 2016 study published in the Journal of Addictive Diseases, 39 percent of daily users met the criteria for clinical insomnia, compared to 20 percent of non-users.
Marijuana has also been linked to potentially serious mental health problems, such as psychotic episodes, major depression and suicidal ideation.
A study published in the May issue of the journal Psychological Medicine found that cannabis use disorders were linked to approximately 30 percent of schizophrenia diagnoses in young Danish men in the year 2021.
Regular cannabis use can disrupt the delicate balance of neurotransmitters responsible for regulating mood and motivation.
Many people who already suffer from depression may self-medicate with marijuana due to its sedative properties, but continued use can have the opposite effect.
As marijuana laws have been relaxed, a black market industry of potent strains and vapes has emerged, with products that offer a high far more potent than the previous one.
Now more than 40 million adults – 16 percent of the population – use marijuana, a rate that has more than doubled in the past decade amid a seismic cultural shift that is creating greater acceptance of medical and recreational use.
