Why are Brits STILL struggling to get a face-to-face GP appointment?
>
Brits are still struggling to get face-to-face GP appointments — despite multiple ministers promising to fix the situation.
Furious campaigners claim patients are being trapped in a ‘Catch 22’ system that bounces them between phone queues and online forms.
And when they do eventually get through, many complain they are still unable to secure an appointment in-person.
One GP practice is still partly blaming Covid for the overall mayhem.
This map shows the 50 GP practices with the lowest proportion of face-to-face appointments according to official NHS data. MailOnline’s analysis excluded practices if the mode of appointment was unknown for more than 20 per cent of their consultations and if the GP service did not routinely offer regular face-to-face appointments, such as care home services. NHS Digital describes this data as ‘experimental’ meaning it may not capture the full picture and is more prone to reporting errors

Patients at Montgomery House Surgery have complained about being trapped between phone queues and online forms while trying to get an appointment, all the while being thanked for their ‘patience’ during the Covid crisis by outdated automated messages
An automated message at the surgery in Oxfordshire thanked patients stuck in a phone queue for their ‘patience’ during the pandemic.
This is despite it being almost a year since all the final pandemic restrictions were lifted.
Since then, several health secretaries have demanded that family doctors — who earn £110,000 on average — return to normal operations.
Patient advocacy groups told MailOnline ‘dehumanising’ tales of patients struggling to see doctors are emerging up and down the country, which give the impression that some GPs ‘do not want to see patients’.
Latest NHS figures on GP appointments show 69 per cent of all appointments were held face-to-face in November.
This was down slightly on the figure for October (71.3 per cent), which marked the highest proportion since the start of Covid.
In-person consultations nosedived during the pandemic, with the rate dropping as low as four in 10 during the early days of the virus crisis as Brits were told to stay at home to limit the spread of the virus.
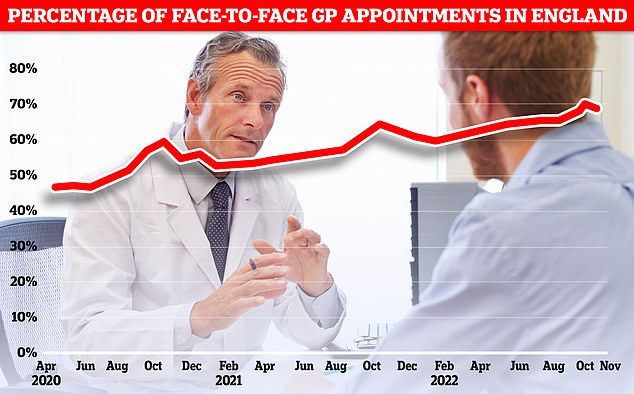
The proportion of GP appointments held face-to-face dipped to 69 per cent in November a slight reversal after months of steady improvement since last February. The figure while higher than the lows of the pandemic is still a far cry from the some 80 per cent of appointments that were held in person pre-Covid
Despite trending upwards in 2022, the proportion of consultations carried out face-to-face is still way below the 80 per cent levels seen pre-Covid.
Top GPs have stated a 50/50 balance of in-person and remote appointments is about right, and that patients shouldn’t get a face-to-face appointment if there is no clinical need for one.
But campaign groups disagree, warning that telephone or online consults are not appropriate for everyone and aren’t always the best way of diagnosing patients.
Dennis Reed, from Silver Voices, a campaign group for senior residents which has repeatedly voiced concerns about GP access in the UK, said a lack of face-to-face appointments remained a constant issue
‘People haven’t seen any discernible improvement in the situation since the end of the pandemic,’ he said.
‘There’s been a lot of good intentions from the Government with a carrot and stick approach but none of it appears to have really scratched the figures.’
He added that despite repeated ‘good intentions’ from ministers, progress on face-to-face appointments was ‘funereal’, with the issue having faded into the background amid the NHS strikes on pay.
Mr Reed said this risked a lower level of face-to-face appointments compared to pre-Covid of becoming the new normal.
‘There doesn’t appear to be any great action on improving the situation with GP appointments and this sort level is becoming ingrained in the figures,’ he said.
Although access to face-to-face appointments have been a huge problem, some Brits are often struggling to get through to a family doctor at all.
The latest tale of GP access woe comes from patients registered with Montgomery House Surgery in Bicester, Oxfordshire.
Patients there claim to have been stuck for days at a time trying to contact their practice for an appointment, rushing to call at 8.30am when the lines open only to be trapped in the queue for hours.
While waiting they are occasionally blasted with the recorded voice stating: ‘Thank you for your patience during the current pandemic.’
Some patients stuck in this maddening loop for over an hour said they then opted to head to the practice itself to see if they could book an appointment in-person.
However, the receptionist then told them to fill out an online form to describe their symptoms that their GP could then look at.
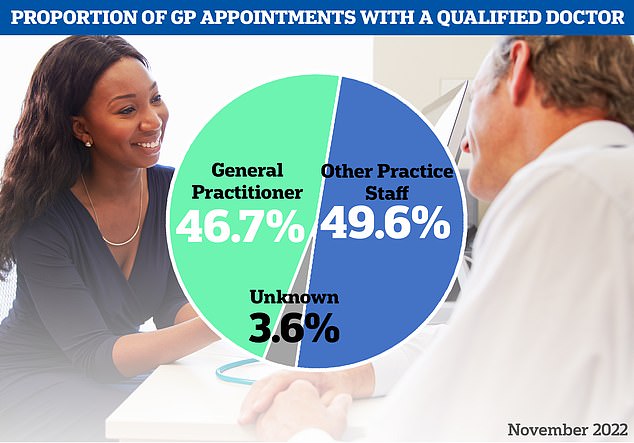
The latest NHS data on GP appointments for November showed the majority of appointments held were not with a family doctor instead being picked up another staff member like a nurse or paramedic
But this left some patients tearing their hair out as, after using the form, they were greeted with the message: ‘We can’t safely assess your symptoms through this online request. You need to talk to someone today instead.’
Mr Reed claimed similar chaos was happening across the country.
‘All of things they’ve described… I hear every day,’ he told MailOnline. ‘People feel that they are just banging their heads against a wall.
‘It’s a Catch 22 situation, you can’t find your way through the system, you turn one corner and there’s another barrier in your way.
‘It gives the impression that certain practices don’t want to see patients.’
He said this process was ‘dehumanising’ for patients because they feel like they’ve become little more than a number in a telephone queue or a code on a form.
‘Patients are increasingly being seen as bundles of data,’ he said.
‘They’re real people who want to talk about their conditions, want some empathy, want to be able to talk to a human being, not have to tap on a keyboard.’
He added that said GPs’ ‘antiquated’ telephone systems needed improvement across the country.
‘The Government keeps promising they’re going to improve the telephone systems, and a lot of them are really antiquated, but I don’t see any signs that things are improving,’ he said.
‘It’s the everyday experience of people trying to engage with GP practices, and something has to be done.’
Healthwatch England, another patient advocacy body, told MailOnline access to a family doctor is the ‘top issue’ people are raising with them.
Louise Ansari, the organisation’s national director, said: ‘People continue telling us about the difficulties they face getting through to their local practice including, long waits on the phone, issues with online booking systems, and a lack of available face-to-face appointments.’
As well as causing frustration , barriers to getting GP appointments could also cause patients harm and put pressure on other NHS services if their condition deteriorates.
‘GP services are often the first port of call for people who need care and so the lack of easy access puts people’s health and wellbeing at risk and increases demand on overstretched hospitals – both from those who cannot get a GP appointment so seek care at A&E, and from people who now need more advanced care and treatment because they were unable to get help sooner,’ she said.
Healthwatch England has called for NHS England to undertake a formal review of GP access to ensure the system works for all patients, including keeping the information they communicate to patients updated.
Rachel Power, chief executive of charity The Patients Association, claimed it had also been told of similar problems.
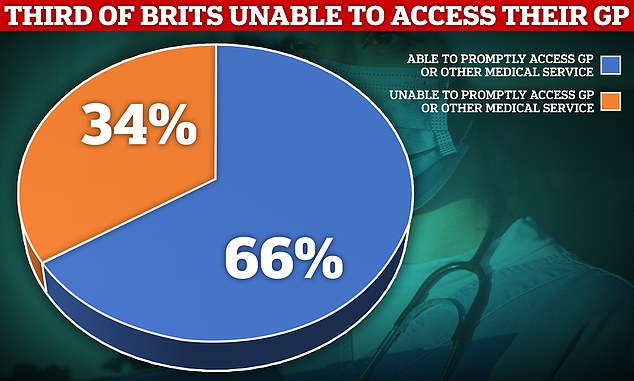
More than a third of patients were unable to access a GP when they needed one in the past year, a MailOnline survey revealed today. The poll of 1,500 Brits showed 34 per cent said they could not get an appointment their local doctor or other NHS services when they tried to in 2022
‘We hear from members they experience difficulties getting through to their general practice and booking appointments that meet their needs,’ she said.
‘This has been going on for a long time and we do not believe it will be resolved until there is a workforce strategy that ensures we have enough doctors and nurses to deliver the care patients need.’
The Patients Association has been calling for extra funding to improve GP telephone services for years, to help family doctors to install extra phone lines and pay for more staff to answer calls to help reduce queues.
‘Improving general practices’ ability to handle calls would reduce patients’ frustration and increase satisfaction with their practices, and probably alleviate pressure on receptionists too,’ she said.
The Government has some plans to enable Brits to book GP appointments without resorting to telephone queues such as using NHS app to let patients book consultations in advance.
Health thinktank, Future Health, added that family doctors are not doing themselves any favours by failing to update pandemic-era messaging.
Richard Sloggett, programme director for the body’s research centre said: ‘Given the pressures facing the NHS it is perhaps not surprising that GP phone systems and websites still contain outdated information and advice on the pandemic.
‘But this poor information creates confusion and wastes time and effort for both patients and busy staff.’
Mr Sloggert added that the Government needed to both update and standardise GP phone systems and booking systems and that it would deliver massive benefits in battling the 8am scramble for appointments for little cost.
‘The technology exists to easily standardise websites and automate information updates. A small investment could deliver a much wider set of benefits,’ he said.
‘It is time to upgrade GP websites and phone systems and create a better front door that works for patients.’
Multiple health secretaries have vowed to drastically boost the number of face-to-face appointments.
Sajid Javid was involved in an ongoing row with family doctors over a lack of face-to-face appointments, at one point blaming it for a the A&E crisis as it left sick Brits with nowhere else to turn to.
And in October 2021 he pledged: ‘I am determined to ensure patients can see their GP in the way they want, no matter where they live.’
Therese Coffey, who was in charge of the Department of Health during Liz Truss’s 49-day tenure as PM, vowed to ease the 8am ‘Glastonbury ticket-esque’ scramble to phone a GP for an appointment.
Her ‘Plan for Patients’ involved new telephone systems to make it easier to get through to receptionists and keep callers updated of their place in the queue.
His successor Dr Coffey, upon unveiling her plans in September last year said: ‘I am determined to make it easier for people to get an appointment with their GP practice when they need one and this will allow patients to make a more informed choice about the care they receive.’
She has since been supplanted by the current minister Steve Barclay, who said in November as he published new GP practice-level data on n face-to-face appointments : ‘I am determined to make it easier for people to get an appointment with their GP practice when they need one and this will allow patients to make a more informed choice about the care they receive.’
NHS data show that 51 per cent of the 8,000 appointments held at Montgomery House Surgery in November were held face-to-face, below the national average.
But the practice didn’t even make it into the 50 lowest performing practices in England by this metric.
Analysis of experimental NHS data found that as few as one in six appointments in some surgeries were held face-to-face in November.
One of the lowest performers overall was Bath Road Surgery in Hounslow, West London, where only 900 of the some 6,000 appointments that month were held face-to-face, a miniscule 15 per cent of the total.
The league table of practice-by-practice data, complied by the health service’s statistics body NHS Digital, was brought in by the Government to effectively name and shame poor performing surgeries as part of a months-long row over face-to-face appointments.
But the experimental data has been described as being of ‘poor’ quality by the NHS’s statistics body meaning it may not capture the full picture and is more prone to reporting errors.
NHS Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board, which is responsible for health service in the area covered by Montgomery House Surgery, was contacted for comment.
A spokesperson for Montgomery House Surgery said: ‘Demand for GP services is high everywhere and practices are doing their best to meet patients’ needs with the resources they have.
‘We know that most of our patients are aware of these pressures and appreciate their understanding and patience as we work to improve our service.’
They added they were monitoring their phone system waiting times and that they had been higher than expected in December due to staff being ill with flu and Covid, and that the practice had recruited more staff to meet demand.
The spokesperson also said the practice has now changed their pandemic automated message, but it was still playing when MailOnline called the practice.
‘Patient care is our priority and we cannot comment on individual cases but encourage patients to feedback their experiences of using services to us directly so that we can review and respond to individual cases,’ they said.
Patients have continually expressed their frustration over a failure of GP services to return to pre-pandemic levels of access, particularly regarding face-to-face appointments.
Despite 80 per cent of patients being seen in-person pre-Covid, top doctors have suggested the figure may never return to this level.
They have said the mixture of in person and remote appointments is balanced and that patients shouldn’t have a face-to-face appointment simply because they would prefer one.
The sector is also being hit by a staffing crisis, with too few GPs for too many patients, especially in some parts of the country.
This crisis is partly being fuelled as increasing numbers of doctors are reducing their working hours and retiring early, while some are leaving to the private sector or abroad because of the pressures.
Doctors’ union, the British Medical Association estimated England is short of about 2,000 GPs, with recruitment failing to keep pace with demand.
Professor Kamila Hawthorne, chair of the Royal College of GPs (RCGP), said family doctors understood their patients’ frustrations in getting an appointment.
‘We understand and share our patients’ frustrations when they are unable to easily access the care and services they need and that we want and are trained to deliver,’ she said.
‘However, hardworking GP teams are being blamed for a situation that is not their fault and beyond their control.
‘Successive governments have failed to sufficiently invest in general practice for over a decade and we are now seeing the consequences, with overstretched and understaffed GP teams trying their best to deliver patient care in extremely difficult circumstances.’
She said that this winter in particular was showing how busy GPs were.
‘This winter, we are the first port of call for the increased rates of winter viruses such as influenza-like illnesses and exacerbation of chronic respiratory conditions, as well as cases of streptococcal tonsilitis,’ she said.
‘This is in addition to delivering vital winter immunisation programmes and delivering interim care to the millions of patients on NHS waiting lists.’
The RCGP has been calling for the Government to implement a new recruitment and retention strategy for GPs in England that goes beyond the 6,000 family doctors pledged by Conservatives in their last election manifesto.
Dr Kieran Sharrock, the British Medical Association’s England GP committee acting chair, also said family doctors are frustrated by the situation.
‘GPs share the frustration of patients when they find it difficult to get through to their practice,’ he said.
‘It is a simple case of demand outstripping capacity, as any receptionist will tell you as they manage the huge volumes of patients calling to book into limited appointment slots daily, creating bottlenecks.’
He said patients were being let down by a lack of a Government strategy to keep family doctors working.
‘With this mismatch it’s regrettable but inevitable that some patients are waiting longer, as practice teams try their best to manage demand and ensure that people who need their care most get it.’
He added that a lack of trained GP practice receptionists was also a factor.
‘Many practices do not have enough receptionists to manage the incoming queries,’ he said.
‘They struggle to recruit and keep these valuable team members due to the extreme pressures of the job and a lack of investment in practices that means they receive better pay elsewhere.
‘So, while we recognise the distress and frustration when people struggle to get through, the abuse that many of our front desk colleagues experience on a daily basis is wholly unacceptable and will only make the problem worse as it drives more to leave.’
A Department of Health and Social Care spokesperson insisted it had been clear that GPs must offer face-to-face appointments and respect patient preferences for them.
‘We are clear that GP practices must provide face-to-face appointments alongside remote consultations, and should respect the preferences of patients unless there are good clinical reasons to the contrary,’ they said.
‘NHS England is accelerating the delivery of cloud-based telephony systems, which will support GP practices in improving call handling and allow them to plan for staffing during busy periods.’
An NHS England spokesperson added: ‘GP teams are working non-stop to get people the care they need, delivering millions more appointments compared to pre-pandemic, with two thirds getting seen within a week and seven in 10 patients getting treated in person.’
Although Covid has faded into the background, the virus can still disrupt GP services.
This can be due to staff needing time off if they fall ill from the virus as well as practice manhours being used to roll-out Covid vaccines.
Within the past few days Mr Javid has repeated his claim that the current NHS model is ‘unsustainable’ and backed calls for radical reforms that would see patients charged for GP appointments.
Former health secretary and veteran Tory Ken Clarke also put forward a similar argument earlier this month.
The latest row over GP access comes after an analysis of NHS data found over five million people a month were unable to book a GP appointment in the year up to October 2022.
It found only a fifth of Britons said they were always able to ‘promptly access’ their GP over the year.
