Weight-loss jabs like Ozempic and Wegovy cut colon cancer risk by half – and increase breast cancer survival by a third, study suggests
Weight loss jabs could spark a ‘revolution’ in cancer care – reducing the number of cases and deaths, leading experts suggest.
Companies such as Ozempic and Wegovy can reduce the risk of obesity-related cancers by a fifth and bowel cancer by half, according to groundbreaking research.
Trial results presented at the world’s largest cancer conference showed that breast cancer patients taking this class of drugs were a third less likely to die five years later.
Doctors say it would be the ‘icing on the cake’ if the drugs, which have been shown to reduce heart attacks and strokes, had a similar effect on cancer.
Significantly, they believe there are “multiple ways” they can help reduce cancer risks, beyond the weight loss they are known for.
Above you see a package from Wegovy. Taken weekly, injections are in short supply in the U.S. for their potential to aid weight loss

Revolutionary weight loss injections such as Wegovy and Ozempic could reduce the risk of some of the most common and deadly cancers (Stock Image)
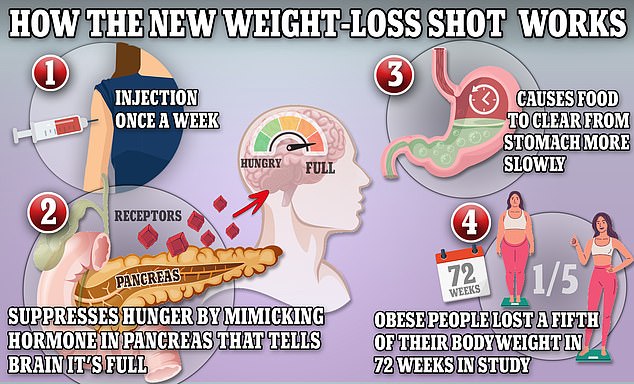
Wegovy and Ozempic work by causing the body to produce a hormone called GLP-1, which is released naturally from the intestines after meals.
The GLP-1 agonists, a new class of drugs that includes Ozempic and Wegovy, were featured in several studies presented at the world’s largest cancer conference.
Scientists from Case Western Reserve University (CWRU) in the US studied data from more than 34,000 obese patients and found that the drugs could ‘delay or prevent’ cancer.
Researchers looked at the 13 different types of cancer with proven links to obesity, including breast, colon and liver cancer.
They found that rates of obesity-related cancer were 19 percent lower in those who took the drugs for at least a year, compared with those who did not.
When other health benefits were taken into account, these patients were half as likely to die over the 15-year period, the study found.
Co-authors Dr Cindy Lin and Dr Benjamin Liu said: ‘To our knowledge, this is the first study of its kind to examine the comparative risk of obesity-related cancers with GLP-1 RAs versus bariatric surgery.
‘Our findings are significant because they could change the paradigm of obesity management by suggesting that early intervention with GLP-1 RAs could delay or prevent the development of obesity-related cancer.’
The results were similar to those who lost more weight through surgery, suggesting that the effects may be due to other factors at play, such as reduced inflammation.
Dr. Mitchell Lazar, director of the Institute for Diabetes, Obesity and Metabolism at Penn Medicine, said in Chicago: ‘Obesity is a risk factor for almost all cancers, in both men and women.
‘The revolution in the medical treatment of obesity thus has enormous potential to prevent new cancers, reduce the severity and growth rate of existing tumors and synergize with new cancer-specific therapies.’
Another Harvard University study presented at the conference looked at 1,448 women with breast cancer and type 2 diabetes, half of whom were taking these drugs.
All received hormone therapies to control their disease, which can cause weight gain, and half also received GLP-1s.
Five years later, the number of deaths appeared to decrease by a third (33 percent). Five years later, the number of heart attacks and strokes also fell by 41 percent.
It comes after CWRU scientists discovered the drugs cut the risk of bowel cancer by up to half in patients with type 2 diabetes.
Researchers looked at more than 1.2 million patients starting diabetes treatment and found that those who were overweight or obese and used the GLP-1 injections, which were initially licensed to treat diabetes, were 50 percent less likely to develop colon cancer develop than patients who used insulin.
While losing weight is known to help reduce the risk, the scientists also observed a 44 percent reduction in all diabetes patients who used the jabs, regardless of their weight.
Julie Gralow, chief medical officer at the American Society of Clinical Oncology (ASCO), said the study was still in its early stages but showed potential for the future.
She said: ‘I think these drugs have so many potential and already proven health benefits that it would be the icing on the cake if we saw them also reduce cancer rates.
“So for the right population, I’m very hopeful about the overall improvement in health from this class of drugs.”
Cancer Research UK’s chief medical officer, Professor Charles Swanton, said: ‘Although GLP1 RAs are effective drugs for managing weight loss, our understanding of the drugs and whether they can reduce the risk of cancer in people is still in its infancy.
He added: ‘Well-designed prospective trials with randomized data will provide further clarity on the potential and safety of weight loss medications to reduce people’s risk of cancer.’
