‘Weight-inclusive’ doctors outraged for refusing to weigh patients for fear of upsetting them
A growing number of doctors across a wide range of specialties have done away with routine patient weighing in an effort to avoid weight shaming, but others argue it obscures a crucial health metric.
Patients are typically weighed as the first step during a routine doctor’s visit.
But the standard practice is increasingly falling out of favor as more people say it makes others feel ashamed about their weight, causing them to run from the doctor even when they have health problems.
It has long been thought that weight is strongly linked to a litany of health problems. So doctors rely in part on the number on the scale to guide their thinking and serve as the building block for a diagnosis.
And pgPeople have been told for decades that obesity can be solved with strong will and strict diets and exercise, and the inability to do so. to fall off is a sign of a fatal personal flaw.
Dr. Pamela Tambini, medical director at Engage Wellness, an addiction recovery center where a patient’s weight is crucial to medication dosing, said weight checks at doctor’s appointments are “more than just stepping on a scale — they are an essential health care tool.”
She added: ‘Weight is a crucial indicator of overall health, especially when it comes to chronic conditions such as diabetes, heart disease and high blood pressure.
“While conversations about weight can feel sensitive, routine weight monitoring remains an important part of preventative care and provides insights that go far beyond the number itself.”
It has long been thought that weight is strongly linked to a litany of health problems. So doctors rely in part on the number on the scale to guide their thinking and serve as the building block for a diagnosis
Many professional medical organizations, such as the American Medical Association, have issued guidelines that minimize the importance of weight and body mass index as important health indicators. Instead, they urge doctors to focus equally on all aspects of a person’s health.
While reducing the focus in exam rooms on what the scale says can make a patient feel more comfortable and willing to continue with preventative care and checkups, pushing it aside can pose more risks than benefits.
Dr. Paul Rosenberg, chief plastic surgeon at the New Jersey Gynecomastia Center, is a big proponent of weighing patients.
Weight checks are critical to assessing whether a patient is healthy enough for surgery.
They help distinguish between excess fat and glandular tissue for procedures to remove excess breast tissue in men.
He said: ‘These statistics can reveal underlying medical conditions including diabetes, high blood pressure and certain cancers. Sudden or unintentional weight changes can be a red flag for things like thyroid dysfunction and heart disease.
‘These routine checks are about prevention and early detection. It’s easy to miss detectable health risks if we completely ignore weight checks or don’t share this information with patients.”
Weight checks are simple, non-invasive tools in a doctor’s diagnostic arsenal. Although indicators such as small irregularities in weight patterns may seem insignificant and can easily be ignored, they can sometimes mask underlying diseases.
‘Don’t Weigh Me Cards’, created by More-Love.org, ask doctors not to weigh patients every time they come in for an appointment unless it is absolutely necessary
Continuous weight monitoring is recommended for timely intervention to reduce the risk of long-term disability and improve patients’ quality of life.
“On the other hand,” says Dr. Courney Scott, an expert in addiction and internal medicine, “abrupt and involuntary weight changes – where one experiences sudden changes in weight – can highlight deeper and more serious problems that require attention at the right time.” need.
“Rapid weight change may be due to underlying factors such as thyroid dysfunction, heart or kidney failure, nutritional deficiencies, and even depression or anxiety that deviate from a person’s normal expectations.”
Nowadays, patients can refuse to consent to being weighed, even handing over business cards with bold letters that say, “Please don’t weigh me unless it’s (really) medically necessary.” “This is an effort by an eating disorder advocacy group to empower patients.
However, many experts say that weigh-ins make patients stronger.
Dr. Scott said: ‘This is made possible by allowing patients to track their weight trends, giving them the upper hand when deciding on dietary changes or even seeking medical advice.’
Weight checks also allow for frank discussions with the doctor about the potential benefits of trying other interventions known to improve cardiometabolic health, such as GLP-1 medications such as Ozempic and Wegovy.
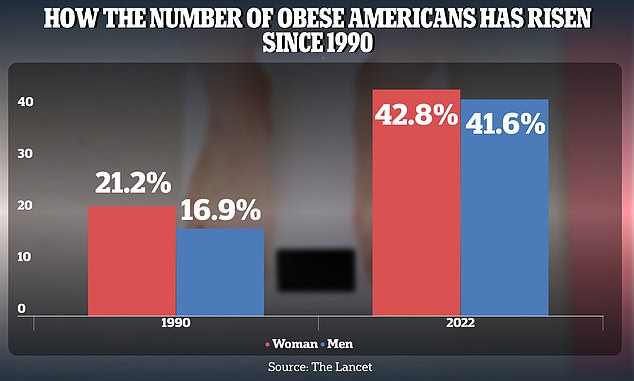
The obesity rate among American adults has increased from 21.2 percent in 1990 to 43.8 percent in 2022 for women and from 16.9 percent to 41.6 percent for men. Obesity is a proven risk factor for a wide range of health problems
Dr. Rosenberg added, “In my practice prescribing GLP-1s and related treatments, I have seen firsthand how powerful it can be to provide information to patients in a respectful manner and in the right context.
‘When patients are informed about their weight and how it relates to their health, they are more likely to adopt strategies to manage or improve it. Avoiding the conversation entirely in the name of preserving mental health may do more harm than good by potentially delaying critical care.”
Obesity is a persistent public health problem in the US, where approximately 40 percent of people are overweight or obese.
Obesity rates were consistently highest among adults aged 40 to 59. Overall, 46 percent of Americans in that age group were considered obese.
It is expected that people with obesity have about 28 percent greater risk of being diagnosed with heart disease, a 24 percent higher risk of stroke and a nine times greater risk of developing heart failure.
When doctors and nurses weigh patients, it is crucial to approach the subject with tact and sensitivity.
Surprisingly, despite the fact that health care institutions are designed to support and promote health, research over four decades shows that individuals with obesity often experience weight stigma and discrimination from health care professionals.
Studies have shown that 69 percent of doctors46 percent of nurses and 37 percent of dieticians show a prejudiced attitude towards people with obesity.
In 2023, experts found that half of approximately 380 women thought this was the case okay to decline to be weighed at the doctor’s office, and almost a third reported having done so in the past due to concerns about weight discrimination based on previous negative experiences with healthcare providers and its negative impact on their mental health.
Dr. Scott said: ‘An important practice that should support this process involves doctors being sensitive to what patients want. For example, aspects such as the feeling of shame and cruelty from focusing too much on your weight can be avoided by choosing not to see their weight, even if the doctors use that data for health purposes.
‘Creating the opportunity to discuss such issues encourages greater focus on trust and requires people’s involvement in caring for their long-term health.’
