US could avert a MILLION deaths each year if mortality rates were on par with 21 richest countries, study
A million deaths in the US could be prevented every year if America’s death rates were on par with those in other wealthy countries, a damning report has found.
Researchers looked at the all-cause mortality rate by population size since the 1930s in almost twenty comparable countries, including Great Britain, Canada, JapanAustralia and 17 European countries.
They found that despite the US being the richest, it has had more deaths per capita than any other country since about 1980, reaching “unprecedented levels” in recent years.
The study finds that the opioid and fentanyl epidemic, gun violence and obesity-related deaths, all of which have been exacerbated by the Covid pandemic, are the reason America is an outlier.
The chart shows how each country in the G7, an informal grouping of seven of the world’s advanced economies, fared in international life expectancy rankings each year between 1950 and 2020. The US fell from 13th to 53rd place.
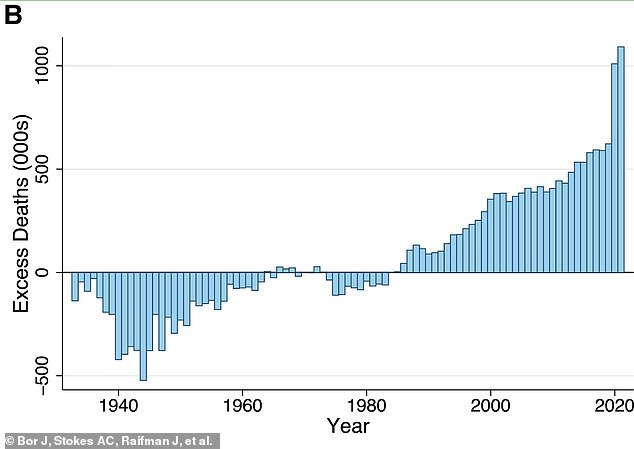
The above graph shows the number of excess deaths in the United States compared to other countries during the period researchers analyzed, from 1933 to 2021. During World War II and beyond, America had a lower death rate than comparable countries. In the 1960s and 1970s the rate was comparable to that in other rich countries. However, in the 1980s the number of excess deaths began to rise
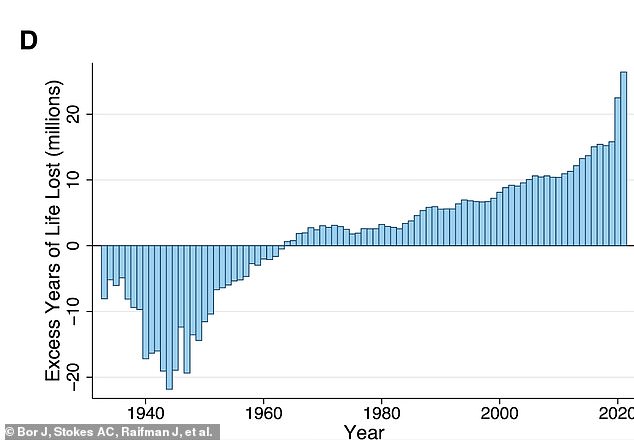
The graph above shows the number of years, in millions, lost due to excess deaths in the US compared to other countries
The study, published in Proceedings of the National Academy of Sciences Nexus, found that about 600,000 deaths could have been prevented in 2019 if the U.S. had similar death rates to peer countries.
But in 2020 and 2021 this rose to 1.1 million.
Steffie Woolhandler, senior author and professor at Hunter College’s School of Urban Public Health, blamed the US health care system, insurers, corporate greed and politicians for the country’s preventable deaths.
“We waste hundreds of billions every year on health insurance company profits and paperwork, while tens of millions cannot afford medical care, healthy food or a decent place to live,” Woolhandler said.
“Americans die younger than their counterparts elsewhere because when corporate profits conflict with health, our politicians side with corporations,” she added.
The United States was just one of a few countries on the list that does not provide universal health care coverage to its residents.
Despite excess deaths peaking in 2020 and 2021, the team from Boston University School of Public Health, University of PennsylvaniaHarvard Chan School of Public Health and Hunter College found that America’s excess mortality rate has worsened since the 1980s.
During World War II and beyond, America had a lower death rate than comparable countries.
In the 1960s and 1970s the rate was comparable to that in other rich countries.
However, in the 1980s, the number of excess deaths began to rise, reaching approximately 622,500 in 2019.
Deaths then rose in 2020 and 2021 during the pandemic. In those years there were about a million excess deaths.
In the years between 1980 and 2021, there were 13.1 million “missing Americans.”
Study leader and corresponding author Jacob Bor, an associate professor of global health and epidemiology at Boston University, called the number of missing Americans “unprecedented in modern times.”
Nearly half of missing Americans died before the age of 65 in 2020 and 2021, a level of excess deaths that Bor said was particularly stark.
‘Think of people you know who died before they reached the age of 65. Statistically, if the US had the death rates of our peers, half of them would still be alive. The US is experiencing a crisis of premature death unique among wealthy countries,” Bor said.
The Centers for Disease Control and Prevention (CDC) reported that life expectancy was 77 years old in 2020, a decrease of almost two years from 2019. In 2021, life expectancy dropped again to 76.4 years.
In 2020, nine of the top ten causes of death were the same as in 2019, although five causes changed ranks.
However, heart disease and cancer remained the top two, while Covid was newly added and took the third spot.
Unintentional injuries moved up to fourth and stroke moved up to fifth.
In 2021, nine of the top ten causes of death remained unchanged from the year before, with heart disease, cancer and Covid once again being the top three.
Unintentional injury and stroke remained the fourth and fifth leading causes of death, respectively, in 2021.
In both 2020 and 2021, deaths among all ages increased year-on-year, except for those among one- to four-year-olds, which only fell slightly in 2020.
“Living in the U.S. is a risk factor for premature death, which is common among many U.S. racial and ethnic groups,” Bor said.
“While most health disparity studies assess disparities among racial/ethnic groups in the U.S., such an approach makes the poor health of whites invisible and grossly underestimates the health deficit of minority groups.
“Using an international benchmark, we show that Americans of all races and ethnicities are negatively affected by the U.S. policy environment, which places a low priority on public health and social protection, especially for low-income people.”
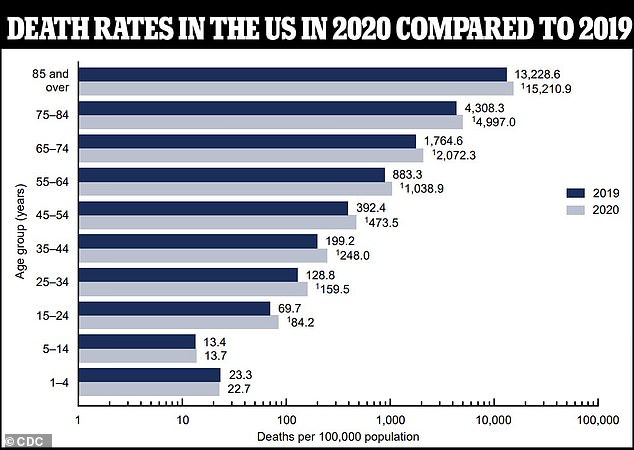
In both 2020 and 2021, deaths among all ages increased year-on-year, except for those among one- to four-year-olds, which only decreased slightly in 2020
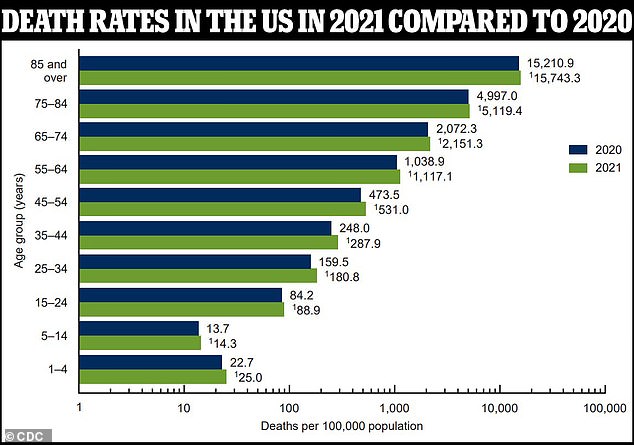
In both 2020 and 2021, deaths among all ages increased year-on-year, except for those among one- to four-year-olds, which only decreased slightly in 2020
Taking into account the future years lost due to premature death, researchers estimate that in 2021 the excess deaths translated into 26.4 million years of life lost compared to comparable countries.
Based on the survey results and the trend of excess deaths in the US, Mr Bor is not optimistic that death rates will recover in the near future, even if Covid deaths fall to some of their lowest numbers.
“The U.S. was already dealing with more than 600,000 missing Americans per year before the pandemic began, and that number was increasing every year. There have been no significant policy changes since then that could have changed this trajectory.
“While COVID-19 has brought new attention to public health, the response that has emerged during the pandemic has undermined trust in government and support for expansionary policies to improve public health.
“This could be the most damaging long-term impact of the pandemic, because expanding public policies to support health is exactly how our fellow countries have achieved longer life expectancy and better health outcomes.”
