The NHS waiting lists hit HARDEST by Covid
>
The number of people waiting for hospital treatment has nearly doubled since the pandemic began among some medical specialties, MailOnline can reveal.
The overall backlog hit a 7.2million in October — the highest figure since records began 15 years ago and two-thirds more than the number logged in March 2020, when Covid first hit British shores.
But our analysis of NHS England figures show the rise is disproportionately spread — with the number in the queue for gynaecology and dermatology treatment almost doubling. This includes procedures such as a hysterectomy and photodynamic therapy, which is used to destroy abnormal cells.
Experts have now called on health chiefs to urgently tackle the disparity, warning some treatments ‘aren’t being prioritised’, which can lead to a declines in patients’ quality of life and mental health, as well as risking infertility in some cases.
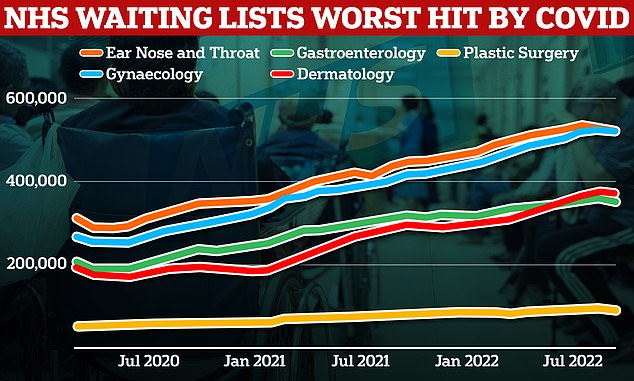
MailOnline analysis of NHS England figures show the rise in the backlog has disproportionately hit some medical areas — with the number in the queue for gynaecology and dermatology treatment almost doubling since the pandemic began. The number of patients waiting for plastic surgery, gastroenterology and ear, nose and throat treatment also jumped by up to 74%
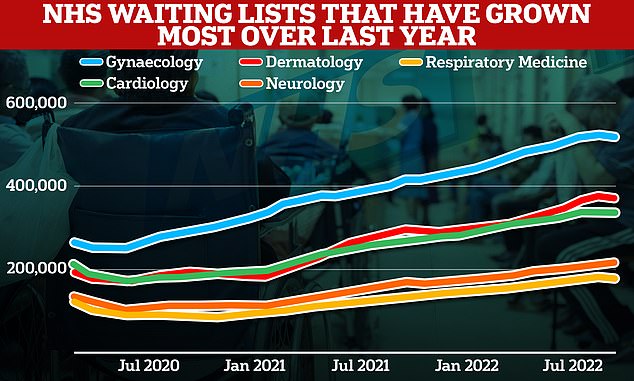
Meanwhile, looking at the latest 12 months, other medical areas have seen the biggest spike in their backlogs. The number of respiratory medicine patients queuing surged 33 per cent, while backlogs in neurology, dermatology, cardiology and gynaecology jumped by up to 29%
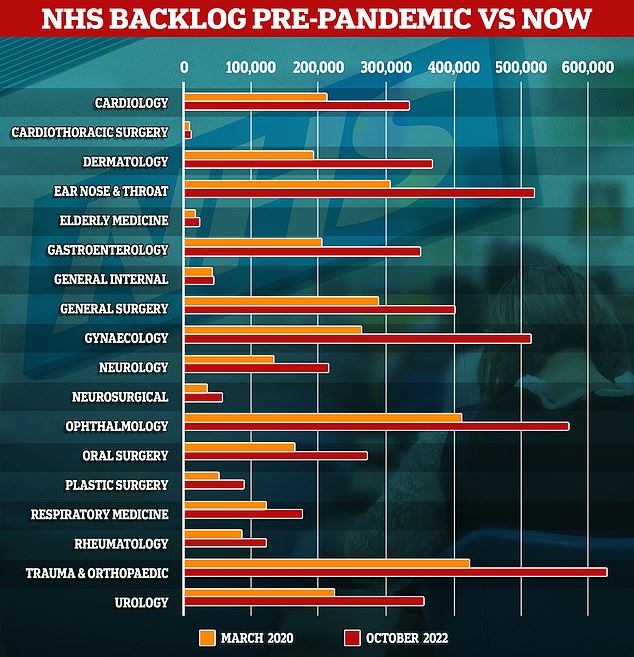
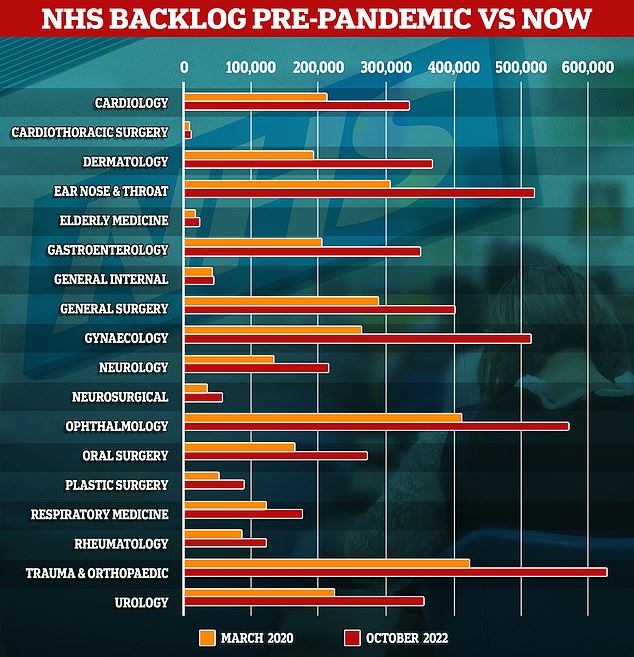
The graph shows the number of people queuing for treatment by medical area in March 2020 (orange), when Covid first hit, compared to latest data from October 2022. Gynaecology, dermatology and plastic surgery saw the biggest rises in backlogs
We examined the NHS waiting list by treatment type since the pandemic began.
This revealed the number of people in the queue for services such as cardiology, orthopaedics and oral surgery per month.
The number of people queuing for gynaecology treatment saw the biggest rise since the start of the pandemic.
In March 2020, 263,280 women were waiting for treatment such as surgery to for endometriosis, fibroids, prolapse and urinary incontinence.
The figure grew by 90,000 in the first year of the pandemic and by a further 100,000 in the second year.
As of October, the latest month backlog figures are available for, 514,604 were in the queue — 95 per cent higher than when the UK was first plunged into lockdown — more than any other medical area.
Dr Ranee Thakar, president of the Royal College of Obstetricians and Gynaecologists (RCOG), told MailOnline that the gynaecological conditions ‘aren’t being prioritised’ and have less access to theatre slots and beds.
She said: ‘Leaving women waiting longer and longer for care often results in increased emergency admissions to hospital or more complex surgery for progressive conditions.
‘More must be done to tackle the unequal growth of gynaecology waiting lists and to meet the needs of women currently on these lists.’
Dr Thakar urged the NHS to rethink how surgical waiting lists are prioritised and consider how queues for gynaecological treatment are impacting quality of life.
She added: ‘We know that for women living with conditions like endometriosis, fibroids, prolapse and urinary incontinence, their symptoms can severely impact their mental health and quality of life.
‘For some progressive conditions, there is also a potential impact on fertility if untreated for longer.’
A report by the RCOG earlier this year found waiting lists for gynaecology services were growing even before the pandemic hit, and had been rising at a faster rate than other specialties since April 2018.
But elective treatment effectively ground to a halt during parts of the pandemic, as the NHS battled against Covid hospitalisations, staff absences and delivered Covid vaccines, creating the biggest backlog ever seen in the health system.
MailOnline analysis also shows that dermatology was also one of the worst-hit services.
In March 2020, 191,559 people were in the queue for treatment for inflammatory skin conditions, such as eczema and psoriasis.
But by October 2022, the figure had hit 371,700 — a 92.1 per cent rise.
Dr Mabs Chowdhury, president of the British Association of Dermatologists, told MailOnline: ‘Dermatology departments across the country are working tirelessly to tackle the backlog of patients waiting to be seen following the pandemic.
‘However, years of workforce shortages, increasing patient numbers since the start of the pandemic, and unprecedented numbers of cancer referrals mean that there has never been a more challenging time for NHS dermatology services.’
Dr Chowdhury, who is also a dermatologist at the private Spire Cardiff Hospital, said the pandemic created a ‘large backlog of patients’ when there was already too few staff and rising demand.
He called for more investment in the workforce, more space for dermatology services in hospital and a better use of telemedicine to reduce ‘unnecessary’ GP referrals. Less than a tenth of those referred for suspected skin cancer actually have it, according to BAD statistics.
The data also reveals that delays to plastic surgery — for treatments such as birth defects, scar and burn reconstruction and hand surgery — have soared 74.3 per cent.
Some 89,940 patients were waiting in October — up from 51,602 in March 2020.
A spokesperson for the Royal College of Surgeons of England (RCSENG) told MailOnline: ‘Unfortunately, the planned waiting list for plastic surgery has grown since the start of the pandemic. The patients who are waiting are typically “category 4” which is “non-urgent routine surgery”.
‘However, for each individual, receiving timely surgery could be life-enhancing and help them to regain their independence, and in some cases, get back to work.
‘A shortage of anaesthetists and nursing staff has had a significant impact on the amount of planned plastic, and other types of surgery that can take place.’
The RCSENG called for a surgical hub in every area of the country to tackle the backlog and give patients ‘the timely treatment they deserve’.
The spokesperson added: ‘That way planned surgery can take place even if there is an increase in admissions to A&E.
‘The Government must also publish its workforce strategy.
‘If we do not have enough staff to meet patient demand, existing vacancies will only get worse, putting remaining staff under more pressure and waits will increase.’
Meanwhile, 204,592 Britons were waiting for bowel, liver and pancreas scans, checks and surgery in March 2020.
But the gastroenterology backlog hit 350,479 in October — a 71.3 per cent rise.
Patients seeking ear, nose and throat care are also some of the worst-affected, with the number in the queue climbing 70 per cent — from 305,057 to 518,803 — over the last two-and-a-half years.
Meanwhile, looking at the latest 12 months, other medical areas have seen the biggest spike in their backlogs.


More than 7.2million patients in England were stuck in the backlog in October (red line)— or one in eight people. More than 400,000 have queued for at least one year (yellow bars)
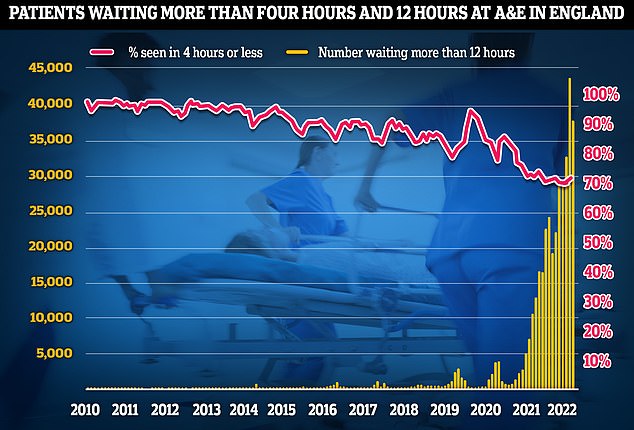
A&E performance worsened in November, with a third of emergency department attendees not seen within four hours (red line) — the NHS’s worst ever performance. Thousands weren’t even seen after waiting in casualty for 12 hours (yellow bars)
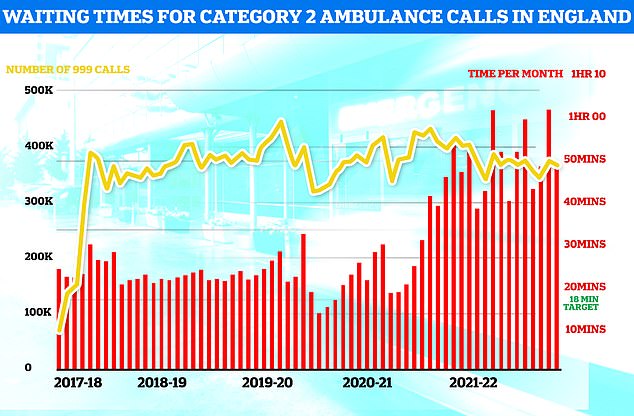
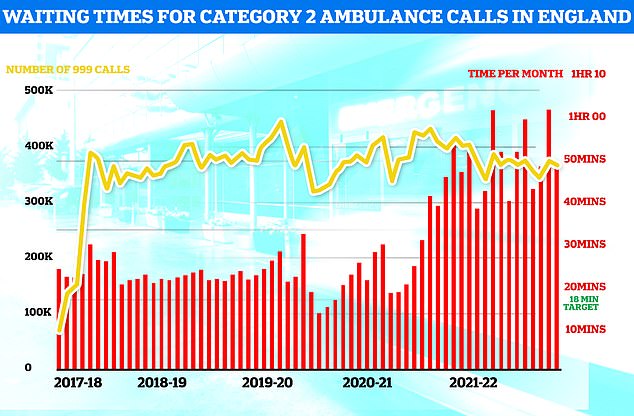
Ambulances took an average of 48 minutes and eight seconds to respond to372,326 category two calls, such as heart attacks, strokes burns and epilepsy (red bars). This is nearly three times as long as the 18 minute target but around 13 minutes speedier than one month earlier
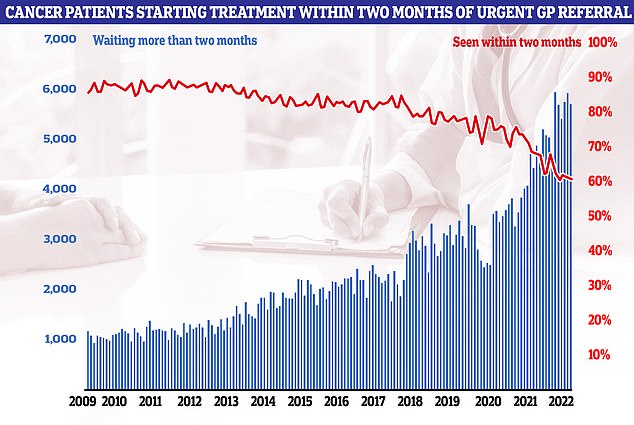
Cancer performance data shows that just six in 10 cancer patients started treatment in October within two months of an urgent referral from their GP (red line). The figure is the second-lowest logged since records began in 2009. NHS targets set out that the figure should be at least 85 per cent. It means 5,728 people waited more than eight weeks to start cancer treatment (blue bars)
The number of people waiting for respiratory care jumped by a third in the year to October — from 131,681 to 175,148 — which marks the biggest surge in the last year.
This is despite the specialism seeing just a 43.5 per cent rise across the whole pandemic — after a high proportion of patients joined the waiting list since last autumn.
Patients stuck in the backlog are waiting for checks and treatment for conditions such as chronic obstructive pulmonary disease and lung fibrosis.
Dr Paul Walker, a member of the British Thoracic Society’s Global Lung Health Advisory group, told MailOnline that the problems are largely down to respiratory specialists being redeployed to deal with Covid patients — leaving the service ‘disproportionately affected’.
He said: ‘Covid is overwhelmingly a lung condition — it causes pneumonia which is lung infection.
‘As such and from the outset respiratory professionals and teams have looked after many more patients with Covid than any other specialty.’
Even when Covid levels have been lower, respiratory teams have been left to look after ‘many Covid patients while other specialties returned to normal’, he said.
Dr Walker, who is also a consultant respiratory physician at Liverpool University Hospitals Foundation NHS Trust added: ‘Hence, the impact of acute Covid was disproportionately much higher on respiratory teams than other specialties and this includes exhaustion and burn out.’
On top of this, ‘many more’ Britons have required respiratory care following the pandemic and specialists have been left to provide Covid follow-up care — such as long Covid clinics — ‘rather than delayed work’, he said.
And the crisis in general practice means there are difficulties providing ‘long-term review and support to many patients’ — leading to a rise in respiratory hospital admissions and referrals, he said.
There is also a severe shortage of respiratory medics, with too few staff to fill vacancies, Dr Walker said.
He added: ‘The impact of these challenges are lower rates of accurate diagnosis, incorrect or missing treatment, worse symptoms and poorer life quality for people with respiratory disease.
‘These people are waiting for clinic appointments, diagnostic tests such as CT scans and lung function tests and in many cases they are waiting for a diagnosis of their lung condition. This potentially delays treatment which will help them feel better.’
Neurology and cardiology backlogs are also among the fastest growing, with the numbers in the queue soaring 28.6 per cent and 24.8 per cent in the last month, respectively.
It comes after latest NHS data shows that an extra 70,000 people joined the backlog in October, taking the queue for treatment to its highest level since records began in 2007.
The data shows 410,983 people had been waiting a year — the equivalent of one in 18 people on the waiting list. The figure is up 1.5 per cent compared to last month.
Ministers have told the NHS to abolish all one-year waits by March 2025.
The number of patients waiting at least 18 months fell by 656 in October. However, 50,124 people were still for one-and-a-half years — a backlog that is supposed to be cleared by April 2023.
Meanwhile, 1,907 people had been waiting more than two years. The NHS had the target of eliminating these long-waiters by the summer.
It says those who are still waiting are either complex cases or have turned down the chance to undergo their procedure sooner at a different hospital.
The NHS says it faces pressure from record demand in emergency care and a surge in influenza cases — with 712 beds taken up by flu patients per day, on average, last week. The figure has doubled since mid-November.
On top of this, 95 per cent of general and acute adult beds were occupied last week, with 13,000 spaces taken up by bed-blockers.
