So much for the world-beating NHS! UK doesn’t even rank in the top 20 for patient safety – and the US scores even lower
Healthcare services in Estonia, Israel and Austria provide safer care than Britain, a report has found.
Researchers from Imperial College London's Institute of Global Health Innovation examined data on 38 developed countries.
The experts focused on four key patient safety indicators for their rankings: maternal mortality, treatable mortality, adverse effects of medical treatment and neonatal conditions.
This includes causes of death that are mainly preventable through timely and effective healthcare, including screening and treatment, and medical blunders.
Norway finished at the top of the rankings, followed by Sweden and South Korea, while Great Britain finished in 21st place and Mexico last.
According to the rankings, the US is in the bottom six.
The analysis shows that 17,356 lives could have been saved in Britain in 2019 if the country had performed at the level of the top 10 percent of countries.
This would have meant 15,773 fewer deaths classified as treatable deaths, 776 fewer newborn deaths, 27 fewer maternal deaths, and 780 fewer deaths due to adverse effects of medical treatment.
Many others survived poor care but suffered from preventable physical or mental disabilities not described in this report, the authors note.
The countries included in the 'Global State of Patient Safety' report, commissioned by the charity Patient Safety Watch, are all members of the Organization for Economic Co-operation and Development.
It says: 'Our country rankings for patient safety highlight existing differences in performance and clear opportunities for shared international learning.'
The researchers warn that without more global collaboration and data reporting, efforts to improve patient safety will be delayed or insufficient, putting harm and lives at risk.
They considered 89 indicators for their report, including the four used to create the rankings, but no country was able to provide them all.
The team calculated the average safety score for all countries and then gave each country a final score based on how much their performance deviated from that average – the standard deviation.
Australia, New Zealand and Norway have the highest availability of patient safety data, with 75, while Britain has 68.
Professor Lord Ara Darzi, co-director of the Institute of Global Health Innovation, said: 'To improve patient safety, we must first recognize that progress is impossible without measurement.
'Our report underlines the urgent need to establish a robust global framework for collecting comprehensive patient safety data, addressing existing data gaps and implementing meaningful indicators.
'Collaboration is the key to progress, and it is imperative that we work together to improve patient safety.
“Patient safety must be evaluated through the lens of the patient, and we must wholeheartedly embrace interventions that include the perspectives of patients, families, and caregivers.”
The authors find that many indicators have shown limited improvement over time, and that there is significant dispersion in performance, even among comparable groups of countries.
A spokesperson for the Department of Health and Social Care said: 'Patient safety is of paramount importance and any death resulting from failings in this area is unacceptable.
'As this report recognises, Britain has taken important steps to improve the safety of care.
'We delivered the first NHS Patient Safety Strategy and appointed the first Patient Safety Commissioner to raise the voice of patients across the healthcare system.
'We have also established a new independent body – the Health Services Safety Investigations Body – to investigate serious patient safety incidents and embed system-wide knowledge, and last week announced a review of the NHS duty of candor.'
Data from HM Treasury shows the annual budget of the NHS. In 2020/21, the NHS received £129.7 billion in core funding for its usual services, supplemented by an additional £18 billion to help alleviate the pressures of the pandemic. For 2021/2022, the Treasury said the health service received £136.1 billion in core funding, as well as £3 billion to help with the Covid recovery. The health sector has been allocated £151.8 billion for 2022/2023 and £157.4 billion for 2023/34. The Autumn Statement added £3.3 billion to these figures each
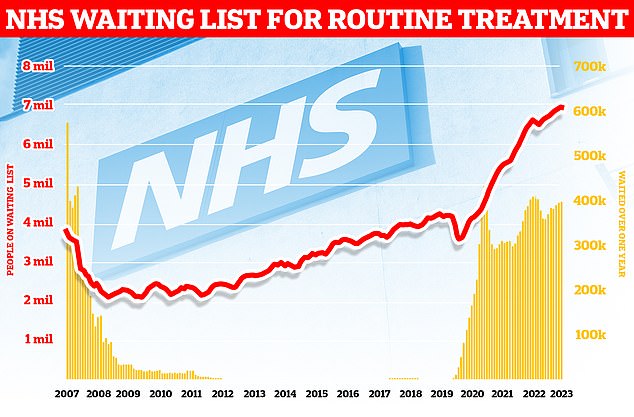
Official figures also show that waiting lists for routine NHS procedures have also risen to a new record, with around 6.5 million patients in England waiting for 7.77 million appointments and procedures in England
James Titcombe, of Patient Safety Watch, became a campaigner for patient safety after his son Joshua died nine days after his birth in 2008 due to failings in his care.
Joshua was one of 11 babies and a mother who died at the University Hospitals of Morecambe Bay NHS Trust for nine years.
Mr Titcombe said: 'Analysis of the data shows that thousands of lives could be saved if the NHS were as safe as the best performing countries and that the NHS in England only ranks 21st out of 38 countries in terms of patient safety.
'This should serve as a wake-up call to the Government and NHS leaders that we must do more to accelerate the pace of change.
“Healthcare systems around the world operate in different and often unique circumstances, but when it comes to patient safety, they are often working to solve similar problems.
'Global collaboration, sharing of data and strategies and interventions adopted to improve patient safety has enormous potential to help transform the pace of progress, not just in Britain but everywhere.
“I hope today's report and the publicly available data platform can act as a catalyst in supporting future efforts to accelerate the pace of progress in patient safety, both here and around the world.”
