Shocking changes coming to GP practices in the new year – as ministers scramble to solve the UK’s sick note crisis
Job Center staff will be based in GP surgeries and physiotherapy clinics in a bid to get sick patents off their benefits and back to work.
The career counselors will encourage unemployed patients to return to the labor market and help them find suitable work.
The NHS will work with the government to trial the program from early next year, starting in areas with high levels of economic inactivity due to poor health.
It will then be rolled out nationally once it is proven to promote wellbeing and tackle the country’s culture of illness.
Amanda Pritchard, CEO of NHS England, said last night: ‘By tackling the rise in health-related economic inactivity and helping people stay in or return to work, the NHS can be a key driver of economic growth. growth in England. ‘
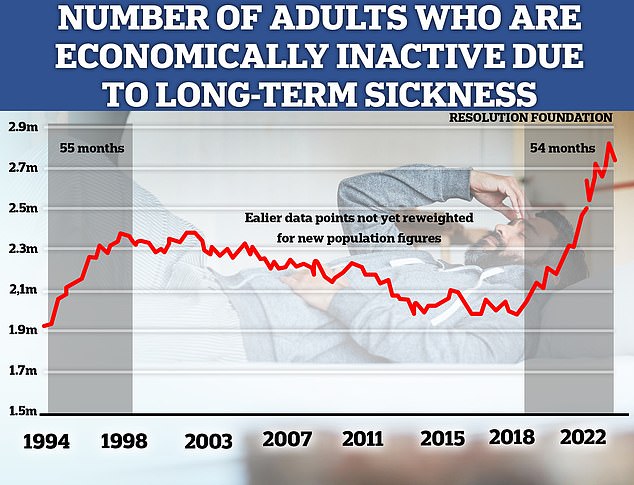
One in ten people of working age – equivalent to 3.9 million adults – now receive health-related benefits in England and Wales.
According to the Institute for Fiscal Studies, this is a 38 percent increase from 2.8 million people in just four years.
During this period, real spending on disability or disability benefits has increased by a third, from £36 billion to £48 billion, and is expected to reach £63 billion by 2028.
Employment Agency staff will be stationed in GP surgeries and physiotherapy clinics in a bid to get sick patents off their benefits and back to work
Backed by £45 million from the Autumn Budget, the trial will see the NHS create ‘Health and Growth Accelerators’ in South Yorkshire, North East and North Cumbria, and West Yorkshire.
The three areas will aim to improve people’s health while tackling the conditions that most impact people’s ability to work, including heart disease, diabetes, back pain and poor mental health.
Staff will step up efforts to prevent the diseases that cause people to lose their jobs, by helping them manage their illnesses and supporting them to make lifestyle changes.
The accelerators, announced at this week’s NHS England board meeting, will also trial the use of phone apps and websites to support mental health and musculoskeletal pain therapy sessions.
Health Minister Wes Streeting has previously promised to reform the healthcare system so it is more effective at getting sick people back to work.
Speaking at an Institute for Public Policy Research event in September, he highlighted how a drop in productivity due to poor health has “cost our economy £25 billion since 2018” and how 900,000 more people are unemployed than before the pandemic would have been the case. trends.
“That’s more people than the staff of Tesco, Sainsbury’s and Asda combined,” Streeting said.
‘If you do nothing, 4.3 million people could be sick by the end of this parliament. Millions of people will be left behind, the social bill will explode and growth will be hampered.’
One in ten people of working age – equivalent to 3.9 million adults – now receive health-related benefits in England and Wales

One in ten people of working age – equivalent to 3.9 million adults – now receive health-related benefits in England and Wales
In addition to the accelerators, NHS England is working with the Office for National Statistics to assess the economic benefits of various health interventions, including talking therapies, bariatric surgery, endometriosis treatment and the NHS Type 2 Diabetes Prevention Programme.
The analysis will cover the impact on waiting times, employment rates and earnings, while incorporating employment from the Office for Budgetary Responsibility and government on labor market impacts.
A pilot project in the North East and North Cumbria, led by the Integrated Care Board and the Department for Work and Pensions, has already helped almost 2,000 people back into work through one-to-one support in County Durham and the Tees Valley.
Samantha Allen, CEO of North East and North Cumbria Integrated Care Board, said: ‘Our GPs often see patients who want to be at work but need practical, non-medical help and also what a doctor can offer.
‘Having a job, a steady income and a feeling of being useful makes a big difference to people’s health – and so far almost a third of patients who consult a consultant have successfully returned to work gone.’
Professor Kamila Hawthorne, President of the Royal College of GPs, said: ‘We know that working in general can be beneficial to the health of our patients, so we are making sure they get the support they need to get back to work going, when it is safe for them to do so, is a good thing.
‘However, it is important that we do not force patients into work or back to work before they are ready, as this could have a detrimental effect on their health.’
Parth Patel, deputy director at the IPPR, said: ‘Most people who are ill would be happy to return to work if they could be better supported.
‘This pilot brings together local health and employment services in a way recommended by our committee report, supported by evidence, to help increase health wellbeing and growth across the country.’
