Scientists hail IVF’s breakthrough in non-invasive tests that could reduce the ‘major element of chance’ involved in getting pregnant
Scientists could be on the verge of a medical breakthrough that breaks the ‘major element of chance’ involved in IVF.
Currently, fertility treatment has a success rate of up to 40 percent.
Academics at the University of California San Diego have now developed a new non-invasive method that can assess the quality of laboratory-cultured embryos.
Currently, fertility doctors usually have to carefully analyze embryos to pick out those with the best chance of success. This may involve taking biopsies or visually assessing them, both of which can be problematic.
The new technology, which is still in its infancy, avoids disruption of the ‘delicate process’.
Currently, fertility treatment has a success rate of up to 40 percent. About a third of IVF cycles among under-35s resulted in a live birth in Britain in 2019. Yet this fell to just 4 percent among those over 44

Academics at the University of California San Diego have now developed a new non-invasive technique that can assess the quality of lab-grown embryos. Currently, fertility doctors usually have to carefully analyze embryos to pick out those with the best chance of success. This may involve taking biopsies or visually assessing them, both of which can be problematic. The new technology, although still in its infancy, avoids interference with the ‘delicate process’
Experts hope it can eventually be “used directly to predict positive IVF outcomes, such as successful births.”
Particles of genetic material, known as exRNAs, remain in petri dishes growing eggs that have been fertilized in the laboratory.
This allows scientists to inspect them without relying on biopsies of the embryos or visual features.
Co-author of the study, Professor Irene Su, who specializes in obstetrics, gynecology and reproductive sciences, said: ‘Unfortunately, IVF success still depends largely on chance.
‘But that’s something we hope our research can change.
‘Right now, the best way we can predict the outcome of embryos is to look at embryos and measure morphological characteristics, or take some cells from the embryo to look at the genetic makeup, both of which have limitations.’
She added: ‘IVF is challenging enough, so it was extremely important to us that our research did not disrupt this already delicate process.
“What we’ve done is more like looking at what was left at an archaeological site to help us learn more about who lived there and what they did.”
The researchers also identified approximately 4,000 different exRNA molecules for each of the five different stages in an embryo’s development.
Using this range of molecules, they could then measure the morphology – the shape, form and structure – of the embryo as accurately as more invasive tests, they said.
Professor Sheng Zhong, an expert in bioengineering from the university’s engineering school, said: ‘We were surprised by how many exRNAs were produced so early in embryonic development, and how much of that activity we could detect using so’ one little monster.
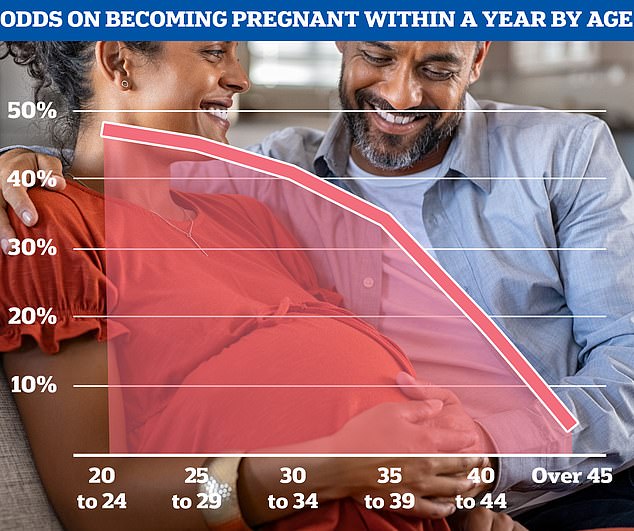
Although conception rates vary for individual women, statistics from the National Institute for Health and Care Excellence show that fertility levels generally begin to decline in the late 20s and then decline rapidly from the mid-30s onwards.
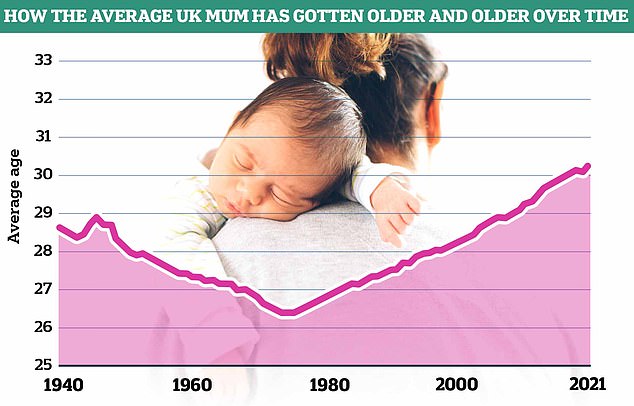
Data from the Office of National Statistics (ONS) shows that the average age of mothers in England and Wales has risen since the 1970s and is now 30.9 years old according to the latest figures
‘This is an approach where we can analyze a sample from outside a cell and gain incredible insight into what’s happening inside.’
Writing in the diary Cell genomicsthe scientists acknowledged that further research is essential to confirm whether their test can be used in practice.
Around 55,000 Britons underwent the grueling IVF process in 2021, according to the latest figures from the Human Fertilization and Embryology Authority (HFEA).
The fertility treatment is often the best method for couples, despite privately costing up to £5,000 for one cycle.
According to the data, success rates ranged from 41 percent for those under 35 to six percent for those over 44.
According to current official guidelines, women under 40 who are struggling to have a child should receive three cycles of the NHS fertility treatment.
But in July, MailOnline revealed that only three parts of the country adhere to these entry criteria, which were developed a decade ago.
The majority of health authorities, who are allowed to set their own entry rules, offer only one IVF cycle.
Some deny it to women over 35 years old. Others even refuse to pay for the procedure if they or their partner already have children.
