There are SIX types of depression, say experts – which could explain why antidepressants don’t work for some
Experts say brain scans show there are six different types of anxiety and depression, a discovery that could lead to better treatments for people with mental illness.
A combination of anxiety and depression is estimated to be the most common mental health problem in Britain, affecting around eight percent of the population, with a similar percentage in the US.
However, many people with the condition are forced to go through various treatments, including psychotherapy and medication, in the hope of finding one that works.
Data shows that as many as four in 10 patients don’t find a treatment that works on the first try, leaving them suffering for longer.
Now a team of American and Australian scientists have used brain scanning technology to find new specific forms of depression and anxiety, in an effort to one day help speed up this process.
A combination of anxiety and depression is estimated to be the most common mental health problem in Britain, affecting around 8 percent of the population, with a similar proportion in the US.
To do this, they collected data from a sample of 1,051 patients with depression and anxiety, 850 of whom were not currently receiving treatment.
Brain scans were taken of patients while they were both at rest and when they were asked to perform an emotional task, such as responding to pictures of sad people.
Experts from the University of Sydney and Stanford University in California then compared these results between the patients and healthy controls to identify any differences.
The aim was to discover whether different parts of the brain ‘lit up’ between patients, showing that parts of the organ behaved differently in some participants.
They also assessed each participant’s symptoms of depression and anxiety, such as insomnia or feelings of suicide, to also identify common symptoms among patients with similar brain scan results.
The end result was that scientists were able to group patients and split depression and anxiety into six different subtypes.
These were called DC+SC+AC+, AC−, NSA+PA+, CA+, NTCC-CA− and finally DXSXAXNXPXCX.
Subtypes were distinguished in the brain scans because certain nerve pathways were hyper- or underactive at rest or responded to certain stimuli.
For example, CA+ (258) patients were found to have a hyperactive cognitive control circuit, the part of the brain responsible for planning and preparation.
While DC+SC+AC patients (169 participants) responded slower than normal when it came to recognizing photos of sad people.
Some also had differences in symptoms. For example, DC+SC+AC+ patients were more likely to suffer from concentration disorders and impulsivity compared to other groups.
On the other hand, NSA+PA+ (154) patients had much more severe anhedonia, which is a clinical term for someone who has a lack of interest, pleasure, or enjoyment in life’s experiences.
In the final part of their study, the scientists also examined whether in patients receiving therapy or medication, one of these drugs proved to be more effective in certain subtypes.
They found that DC+SC+AC+ patients responded better to behavioral treatment, such as cognitive behavioral therapy (CBT) offered by the NHS, compared to the other subtypes.
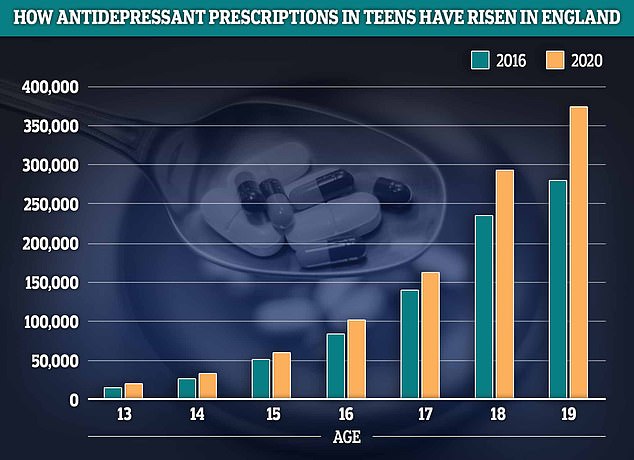
Prescriptions for antidepressants among teenagers rose by a quarter in England in 2020 compared to 2016. The biggest growth was seen among 13 and 19-year-olds, where prescriptions rose by around a third
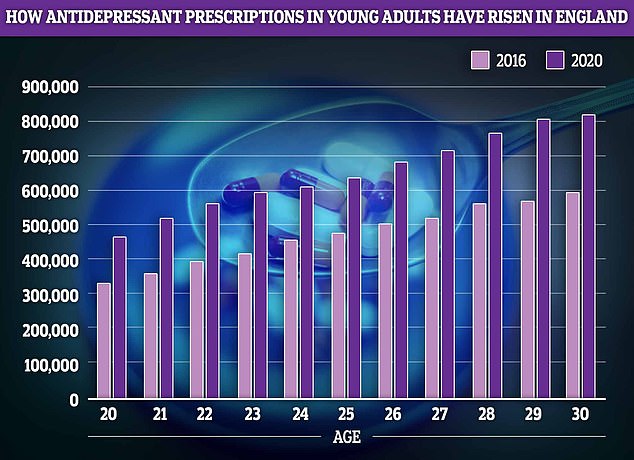
Young adults, who are often leaving home for the first time and starting their careers, also saw an approximately 40 percent increase in prescriptions for antidepressants
This was especially the case for AC patients (161), who responded worst to behavioral therapy of all groups.
Another important difference noted was that CA+ patients had a better response when prescribed the antidepressant venlafaxine.
Authors of the study, published in Naturopathysaid that finding more specific diagnoses for depression and anxiety and, by extension, which treatments would be more effective for each type would improve outcomes for patients.
‘The dominant ‘one-size-fits-all’ diagnostic approach in psychiatry leads to trial and error through treatment options, which is lengthy, expensive and frustrating, with 30-40 percent of patients not achieving remission after trying one treatment,” they wrote.
While they claimed their results were promising, they said they should also be approached with caution and that other studies should replicate their findings.
Other experts have been concerned for years about the “one size fits all” approach to patients suffering from depression.
These concerns have mainly centered on the use of a type of antidepressant called selective serotonin reuptake inhibitors (SSRIs), taken by millions of people, and its libido-crushing side effects.
Some users have reported turning into “sexless” zombies even years after they stopped taking the mind-altering pills.
Use of the pills has soared in recent years, despite growing discomfort among experts about the drugs’ effectiveness in treating depression.
Some research has even suggested that they could increase the risk of heart problems in young people or even, paradoxically, increase their risk of suicide, in addition to the problems of sexual well-being.
However, such research is not unambiguous. Other experts point out that such trends may be due to the patients suffering from the depression the drugs are intended to alleviate, rather than the medication itself.
And many people who use them claim they work.
It is believed that people with depression have low serotonin levels, although there is scientific debate about this, and SSRIs combat this by increasing these levels.
However, some experts suspect that the drugs may cause too much serotonin to be released, affecting people’s health.
Psychiatrists advise patients who are concerned about the side effects or possible side effects of antidepressants to talk to their medical professional about their options.
Doctors may sometimes prescribe an alternate dose, a different medication, or a different medication to combat the side effects.
They urge patients taking these medications not to stop without first speaking to the medical professional responsible for their care, to ensure they are adequately supported.
