Rise of perma-LIST: Thousands of people may already have an incurable fungal infection, as experts find reason for resistant cases to increase
Millions of women in Britain are suffering the pain of repeated attacks of vaginal thrush and many of them cannot be cured, experts warn.
In one study, researchers examined swabs from patients who had experienced at least four episodes of the fungal infection – classified as recurrent – within 12 months.
Of these, 15 percent were found to be resistant to the most powerful first-line treatment, fluconozole, and other powerful antifungals.
It means that in some of these cases the infection is virtually impossible to treat, meaning women may have to rely on medications to keep symptoms at bay for life.
Overuse of common antifungal medications could be the cause, said the scientists behind the study, published in the journal Sexually Translied Infections.
Vaginal thrush is common; three in four women of childbearing age are likely to suffer from it
White discharge, pain and itching around the vagina are all telltale signs of a yeast infection
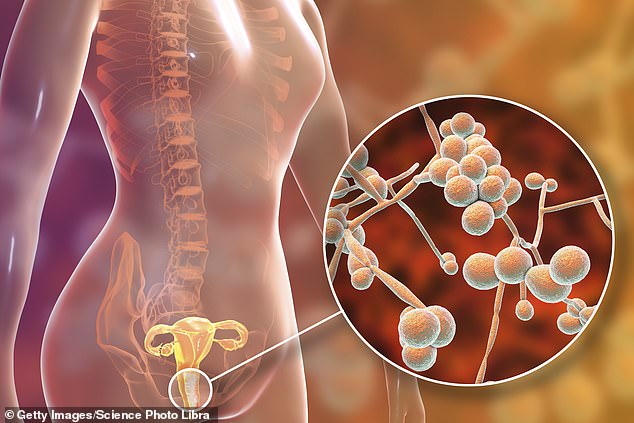
Thrush, also known as candidiasis, is caused by a type of yeast called Candida.
Normally this lives harmlessly in the body, but sometimes it can get out of hand and damage healthy tissues.
The infection can affect the mouth, throat, penis and vagina and causes itching, irritation, pain and sometimes discharge in women.
In recent years there has been concern among skin specialists that some cases are becoming increasingly difficult to treat, with patients regularly having to undergo treatments for months rather than weeks.
Just as harmful bacteria have become immune to common antibiotics, a similar pattern emerges with fungal infections.
To understand the scale of the problem, researchers examined laboratory results from thousands of British women with recurring yeast infections between 2018 and 2021.
The majority appeared to be caused by Candida albicans, the fungus usually responsible for vaginal thrush.
But there was a year-on-year increase in other Candida species, the most common of which was Nakaseomyces glabrata, a species resistant to standard treatments.
In 2018, approximately one in twenty cases was due to these ‘other’ species, rising to one in ten in 2020.
In total, three percent of cases were found to be resistant to one or more standard drugs, including fluconozole, rising to almost 10 percent in 2020.

Fluconazole is used to treat vaginal thrush, but resistance to the antifungal drug has quadrupled in the past three years
‘The increase in non-albicans species is of clinical importance, as some have intrinsically reduced susceptibility to fluconazole,’ researchers emphasized.
‘Successful treatment of fluconazole-resistant Candida albicans and non-albicans species can be challenging and often requires multiple courses of antifungal agents.
“Many of these yeasts also had reduced sensitivity to (second-line drugs) itraconazole and voriconazole, further limiting treatment options,” the researchers added.
Since 2013, the UK primary care guideline recommends that a clinical diagnosis of acute vaginal thrush be made based on the typical signs and symptoms, such as itching and discharge.
Doctors can also test vaginal pH for signs of a yeast infection and follow it up with treatment such as a single dose of oral fluconazole or clotrimazole pessary, a tablet inserted vaginally, researchers say.
But there is evidence that vaginal thrush is being overdiagnosed by both doctors and patients, and researchers suggest this may lead to unnecessary use of antifungal treatments, which may have led to the development of resistance.
The researchers said: ‘The exact reasons for this increase (in fluconazole resistance) remain unclear, but it follows the introduction of limited access to fungal cultures for the diagnosis of (vulvovaginal candidiasis) by those working in frontline care.
‘Instead, a clinical diagnosis is recommended, followed by empiric treatment. Therefore, we believe that this policy of encouraging empiric treatment of vaginitis, based on non-specific symptoms and signs, should be revised.”
