Revealed: How hospitals use ‘underqualified’ doctors to treat the seriously ill and pregnant women because there aren’t enough real doctors
Hospitals are breaking NHS rules by allowing staff with just two years’ training to treat pregnant women and stroke victims instead of doctors, The Mail on Sunday has revealed.
In a move described as a “huge potential threat to patient safety”, a number of NHS hospitals are routinely using physician associates (PAs) to take over the services of doctors.
A PA is an NHS worker without a medical degree who is only meant to assist doctors and nurses. They are not qualified to diagnose patients, prescribe medications or order scans, and are meant to be supervised by a doctor.
But research by this newspaper has revealed dozens of cases in which hospitals have used PAs to fill the shortage of doctors in departments such as gynecology and emergency care.
This is against NHS guidelines.
In 2022, Emily Chesterton, 30, died after a PA failed to spot a blood clot. The actress was seen twice by a PA, who told her she was suffering from anxiety and long Covid
In one of the most concerning cases, PAs have covered for doctors in the stroke unit at Blackpool Victoria Hospital 14 times since the start of the year. According to a Freedom of Information request, the hospital has also allowed PAs to cover for doctors in the emergency department.
Last year, the same stroke unit was hit by a scandal when a nurse and a junior colleague were convicted of illegally administering sedation to patients.
There is also a murder investigation after a patient in the ward bled to death from internal injuries after being attacked by an unknown member of staff. Six years later, police have still not been able to identify the suspect.
There is no evidence that these crimes were committed by PAs or that they occurred during shifts when these non-medical personnel were present.
Following our findings, the family of a woman who died due to errors made by a GP practice nurse has urged the NHS to stop using underqualified doctors to fill the doctor shortage.
In 2022, Emily Chesterton, 30, died after a PA failed to detect a blood clot. The actress was seen twice by a PA, who told her she was suffering from anxiety and long-Covid.
Her parents say that at no point during the appointment was Emily told that the person she was seeing was not a family doctor. A coroner concluded that Emily should have been immediately referred to a hospital emergency room.
The GP practice in North London where she worked has now decided to stop employing PAs.
“It’s terrifying to think that people in hospital are being treated by people they think are doctors but who are really just assistants,” said Emily’s mother Marion Chesterton, a 65-year-old retired teacher from Salford.
“We lost our daughter due to mistakes made by a PA who was not qualified to diagnose her. The fact that hospitals continue to allow PAs to operate in this manner shows that lessons have not been learned.”

Emily’s parents say that at no point during the appointment was Emily told that the person she was seeing was not a family doctor.
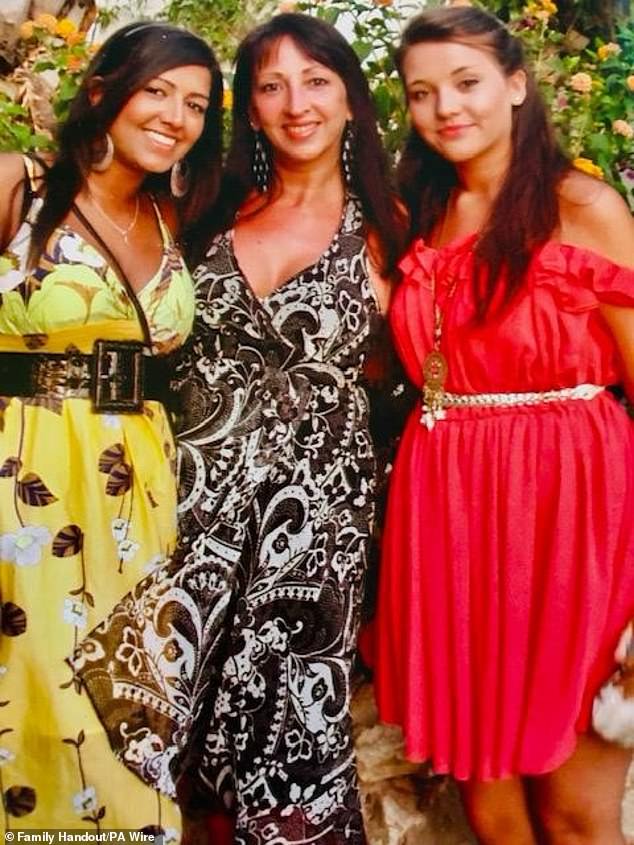
Emily pictured with her mother Marion and sister Jasmine, left
The NHS plans to recruit around 10,000 PAs by 2038 to help ease the doctor shortage.
Last night, NHS England criticised the trusts named in our investigation. ‘There should never be circumstances where physician associates replace doctors,’ a spokesperson said. ‘We are following this up with all the trusts involved. The NHS has always made it clear that PAs are not a replacement for doctors.’
The doctors’ union the British Medical Association (BMA) has urged new Health Secretary Wes Streeting to take action. “These reports confirm that PAs have been deployed in place of doctors on medical rotas at hospitals across the country,” said BMA Council chairman Professor Phil Banfield.
‘This practice poses a huge potential threat to patient safety and is a cause for national concern. PAs do not have the rigorous medical training or qualifications to take on the responsibility of a doctor for patient care, in these trusts or anywhere else.’
He added: ‘While PAs can play a useful role in assisting the wider medical team, NHS England itself has repeatedly told hospital trusts that PAs should not be used as a replacement for doctors in any service. It is inexcusable that these trusts are using PAs in this way.
‘Now that the previous government has failed to take action, it is essential that the new Minister of Health tackles this practice and puts an end to it.’

Protesters gather outside parliament to protest the transfer of responsibilities to junior doctors who have limited medical training and are not doctors

The protesters argue that using medical assistants instead of doctors could potentially be dangerous to patients and lead to loss of life.
The Mail on Sunday was the first to raise the alarm about PAs last year and has been campaigning to rein in The Physician Associates. We believe there should be strict limits on what PAs can and cannot do.
In response to growing concerns, NHS England issued new guidance in March stating that ‘PAs should not be used as a replacement for doctors on a rota’.
But last month we revealed that the Royal Berkshire Hospital had deployed PAs to cover emergency department doctors’ shifts more than 70 times in the past six months, including 21 times since March.
The hospital also repeatedly asked PA students, who had not even completed their two-year training, to replace doctors.
Following these revelations, we have sent Freedom of Information Act requests to all hospital organizations in the country, asking them to disclose when they have deployed PAs to take over the services of physicians since December 2023.
More than 100 NHS trusts responded. The vast majority did not use PAs in this way, and several responded in strong terms, distancing themselves from the practice.
Maidstone and Tunbridge Wells NHS Trust said it would ‘not ask a PA to fill vacant places in a medical service’.
Mid Cheshire Hospitals NHS Foundation Trust said it does not use PAs to fill gaps in doctors’ rosters because ‘they cannot prescribe or request X-rays’.
However, not all trusts shared this attitude. Between December 2023 and May 2024, Northampton General Hospital NHS Trust asked PAs to cover doctors’ services on 25 occasions, mostly in the emergency department. The trust, which employs eight PAs, admitted it was given the services because ‘there was no doctor’s cover available’.
London North West University Healthcare NHS Trust reported that its 37 residents had covered for doctors 76 times in the same period, but it did not specify in which departments these shifts took place.
Barts Health NHS Trust in east London has placed PAs in junior doctors’ A&E services 20 times in the past six months. Four of these cases came after NHS trusts were told to close down the practice. A spokesperson said: ‘Physician associates play a vital role in the care of patients in our hospitals, and we employ 16 of them alongside our 2,500-strong medical workforce.
‘Their job description is clearly defined and is in line with their education, experience and qualifications. In addition, they always work under the supervision of experienced doctors.’
According to Shrewsbury and Telford Hospital NHS Trust, PAs were approached ‘to fill a gap in the timetable’ and ‘cover some aspects of the on-call team rather than leave a gap’.
The foundation argued that not filling a vacancy would “negatively impact patient care” and that it would take too much time to “determine the number of shifts filled by physician associates.”
And Rotherham NHS Foundation Trust cited five instances where doctors’ services were replaced by PAs, all in the gynaecology department.
A spokesperson said: ‘PAs carry out a range of duties within their remit, always ensuring patient safety. All care involving PAs is overseen by qualified gynaecologists to maintain the highest standards of medical care.’
Dr Helen Fernandes, chair of the Doctors’ Association, which represents NHS clinicians, said: ‘PAs should not replace doctors in any area.’
A Department of Health and Social Care spokesperson said: ‘Medical assistants play an important role but should always work alongside doctors and not replace them.
‘If we fix the NHS, we will solve the staffing crisis and deliver the NHS long-term plan, ensuring patients are always cared for by the right, qualified healthcare professional.’
Each hospital mentioned was contacted for comment.
According to the British Medical Association, the NHS has a shortage of almost 9,000 doctors.
