Researchers use Artificial Intelligence to identify potential vaccine for STD that infects 700k Americans each year
Artificial intelligence (AI) could pave the way for a vaccine against gonorrhea, researchers say.
The sexually transmitted disease worries doctors because the disease is resistant to almost all antibiotics. Experts fear that if a super strain gains a foothold in the US, they may no longer be able to treat it.
But researchers from Massachusetts and Denmark say they have used AI technology similar to facial recognition to detect two antigens on gonorrhea that could be used to develop a vaccine to protect against the STD.
“That was really a surprise,” said author Sanjay Ram, an infectious disease expert at UMass Memorial Medical Center.
“No one could have predicted that these two proteins, which were not thought to be exposed on the surface, would work in vaccines.”
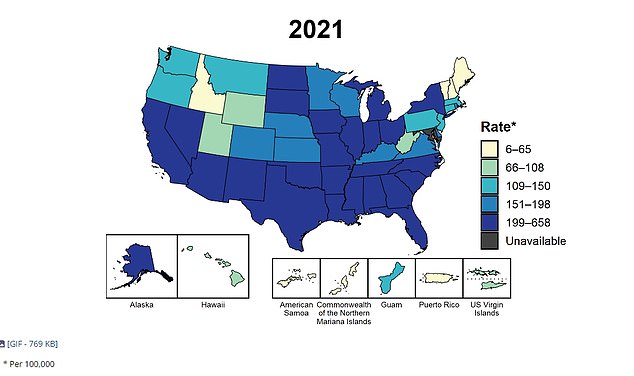
The above map shows cases of gonorrhea in the US in 2021
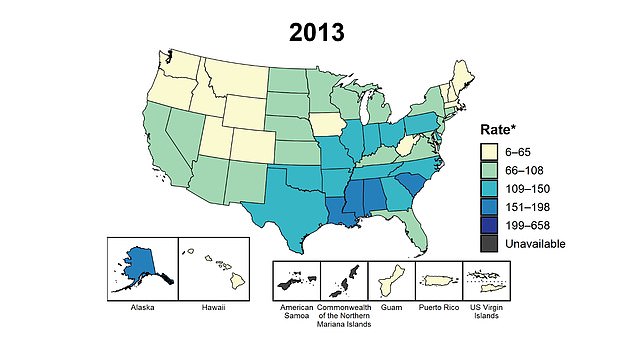
The map above shows gonorrhea rates in 2013 and shows how the number of gonorrhea cases is rising significantly nationally
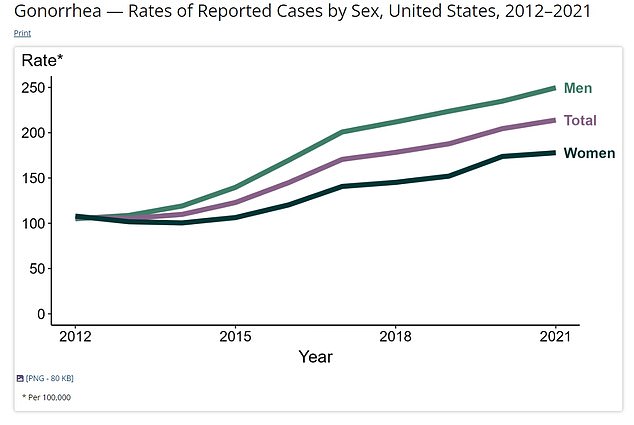
The above shows how cases of gonorrhea are trending upward in men and women, but at higher rates in men.
In the study, published Tuesday in the journal mBioscientists fed AI data into proteins from gonorrhea.
The AI, called Efficacy Discriminative Educated Network (EDEN), uses a feature similar to facial recognition technology to understand the difference between proteins, says Andreas Holm Mattson, the founder of AI immunology startup Evaxian.
The technology analyzed different combinations of proteins from the surface of gonorrhea to suggest the best formula for a vaccine.
Scientists then immunized mice with 11 combinations of two to three antigens recommended by the AI.
The mice were then bled and exposed to gonorrhea in the laboratory to measure the immune response.
After testing, EDEN determined that the proteins FtsN and NGO0265 performed best.
FtsN is involved in the division of gonorrhea cells. Scientists are unsure of the role of NGO0265, but say it is also displayed on the cell surface of gonorrhea.
The researchers then combined the two proteins into a chimeric protein – a protein created by joining two genes – that induced a similar immune response.
About 700,000 Americans get gonorrhea every year, according to statistics from the Centers for Disease Control and Prevention (CDC).
Gonorrhea infections reached record levels in the 1970s and 1980s, with around 400 cases per 100,000 people at their peak.
But with the advent of technologies like condoms, increased awareness of STDs and infection control programs, annual infections have fallen by 74 percent since 1996.
However, in recent years, infections have increased again, with factors such as having more sexual partners, less frequent use of condoms, a lack of testing and the rise of antibiotic resistance all contributing to the increase.

Earlier this year, signs were put up in twenty American cities warning people about the dangers of gonorrhea infections
People can become infected with gonorrhea through vaginal, anal, or oral sex only if the bacteria is passed on through bodily fluids from an infected person.
Early warning signs of an infection include experiencing pain while urinating, having an abnormal discharge from the penis or anus, and redness or swelling in the urethra or vagina.
Infections are treated with a course of antibiotics. But in recent years, with the rise of antibiotic resistance, doctors have begun to warn that an alternative is needed.
If left untreated, long-term gonorrhea infections can increase the risk of complications during pregnancy, such as low birth weight, and increase the risk of other STDs such as HIV by making it easier for the virus to enter the bloodstream.
In some cases, infections can lead to infertility in men due to the formation of scar tissue in the urethra, which can reduce the number of sperm leaving the body during ejaculation.
In women, the bacteria can travel through the cervix to the upper reproductive organs, leading to inflammation and scarring, which can affect fertility.
Earlier this year, two people in Boston were diagnosed with a ‘worrying’ form of super gonorrhea.
There was no connection between the pair, indicating that the superspecies is more widely circulating in the community.
Dr. Margaret Cooke, head of the Massachusetts Health Department, said the discovery was a “serious public health concern.”
In addition to Boston, the strain was previously diagnosed in Britain and Austria.
