Nearly 250,000 more deaths in Britain than in European neighbors in past decade as report blames NHS delays and failures in cancer and dementia care
According to a report, around 240,000 fewer people would have died in Britain over the past decade if avoidable mortality had been at the same level as European levels.
Long wait times for health care and a failure to tackle obesity, couch potatoes and smoking have fueled the deaths, the Institute for Public Policy Research says.
The think tank found that the quality of care nationally has worsened despite increased spending, forcing the country to “spend more to get less.”
Meanwhile, Britain continues to lag further behind other developed countries, with cancer survival rates in particular ‘stubbornly lower’.
The IPPR warns that this trajectory is ‘clearly unsustainable’ and calls on the government to take urgent action to deliver better value for money to taxpayers.
“We estimate that if Britain had had a preventable death rate similar to that in comparable European countries, around 240,000 fewer people would have died in the ten years from 2010,” the IPPR said (shown in chart).
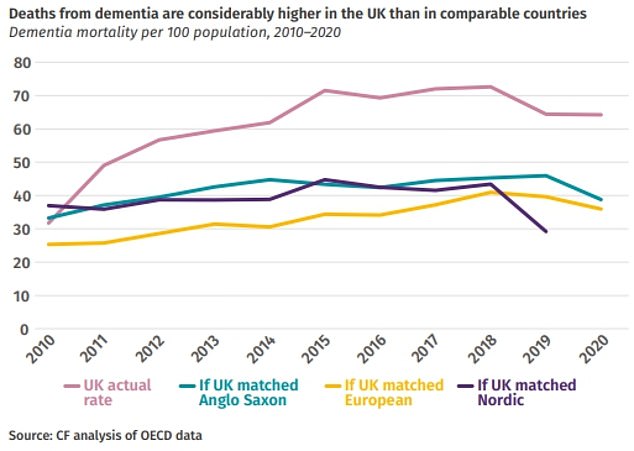
The audit found that Britain’s cancer survival rate is lower than almost all other advanced economies, while the number of deaths from dementia is ‘radically higher’ (shown in graph)
Reforming the NHS to change it from a ‘disease service’ to a ‘prevention service’ would ‘avoid killer costs’ and end ‘second-class care’, it adds.
The new 90 page report comes after the IPPR Commission on Health and Prosperity carried out an audit of health and care services.
It found that poor health costs both lives and lives.
Long-term absenteeism has become a ‘serious budget threat’, with the number of people out of work due to ill health at a record high of 2.6 million.
The report says: ‘There is no path to prosperity for this country without tackling the wave of disease head-on.
‘The number of deaths that could have been prevented by timely healthcare or public health interventions is much higher in Britain than in all other comparable European countries.
‘We estimate that if Britain had had an avoidable death rate similar to that in comparable European countries, around 240,000 fewer people would have died in the ten years from 2010.’
The audit found that Britain’s cancer survival rate is lower than almost all other advanced economies, while the number of deaths from dementia is ‘radically higher’.
British patients are less likely than patients in other countries to be involved in decisions about their care or have less time with their doctors.
And fewer than one in six patients with a preferred GP receives continuity of care.
Furthermore, the communication skills of British GPs are said to have moved from being ranked among the best in the developed world to ‘near the bottom of the pack’.
It comes as patients face a scramble for GP appointments at 8am, practices have yet to return to pre-pandemic levels of face-to-face consultations and NHS waiting lists are at a record 7.6 million people to stand.
The report notes that claims for adult social care have increased by 10 per cent since 2016, but the number receiving local authority support has fallen by 4 per cent.
And almost six in ten people aged 17 to 24 with a suspected mental disorder do not receive healthcare treatment.
Dr. Parth Patel, lead author of the report and NHS doctor, said: ‘We are spending more years with illness than ever before, but it has never been harder to access timely healthcare.
‘The NHS, not so long ago leading the world, has now fallen far behind its international peers.
“With political will, this country’s health care services can once again lead the world.”
On the post-pandemic trajectory, public health spending in England is on track to rise from 9 percent of GDP to 11.2 percent of GDP by 2033/34.
However, the IPPR says its reform proposals could save taxpayers up to £205 billion over the next decade – with annual savings worth the equivalent of the current UK defense budget in 2033/34.
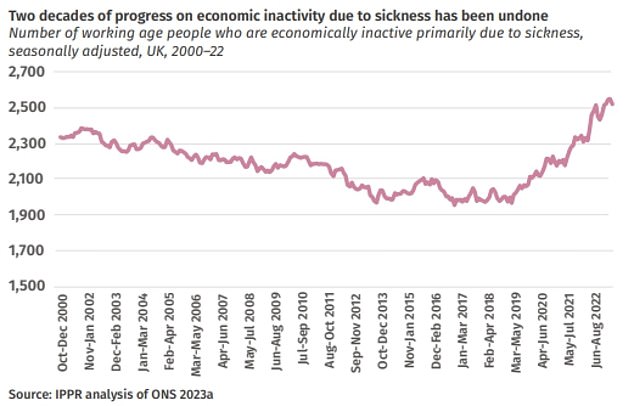
Long-term absenteeism has become a ‘serious budget threat’, with the number of people out of work due to ill health at a record high of 2.6 million. The report says: ‘There is no path to prosperity for this country without tackling the wave of disease head-on’
The ideas include offering a wider range of healthcare services at GP practices, making personal care free so dementia patients don’t have to bear ‘catastrophic’ costs and canceling student debt for health and care workers to make the jobs more attractive.
Lord Ara Darzi, co-chair of the IPPR Commission on Health and Prosperity and former Secretary of State for Health, said: ‘The NHS and social care system are vital to our individual and national health and prosperity.
‘Too many people struggle to receive high-quality care when they need it most.
‘As a result, calls for our ‘free when you need it’ system are increasing.
‘But this is not the time to abandon the principles that underpin the NHS.
‘Instead, we must renew and expand them to achieve better health, a stronger economy and a fairer society.
‘This report sets out a plan to achieve this.’
Lord James Bethell, a former Conservative health minister, said: ‘Sick Britain is costing us our lives and livelihoods and damaging the British economy.
“If we want to change course, we have to stop pretending that the solution is always more hospitals and more acute staff.
“Instead, we must take action to reduce the demand and need for health care through prevention.
‘A mission for a healthy Britain, addressing the simultaneous epidemics of obesity, gambling, addiction and online harm, is a prerequisite for any sustainable, effective National Health Service in the 21st century.’
Fiona Carragher, director of research and advocacy at the Alzheimer’s Society, said: ‘This report highlights the serious consequences of failing to invest properly in health and social care.
‘If Britain had matched the dementia death rates of our European counterparts, 180,000 people might not have died from dementia between 2010 and 2020.
‘We greatly welcome the pragmatic and constructive recommendations from the IPPR report on healthcare reform, from a social care guarantee that will provide free personal care and raise the quality of healthcare providers through ethical commissioning, to a new deal for health and care workers that paid all healthcare workers the real living wage and received appropriate training and support for their role.’
Matthew Taylor, chief executive of the NHS Confederation, which represents healthcare organisations, said: ‘Investments that keep people out of hospital and prevent ill health will save money in the long term, support the economy and help secure a sustainable, prosperous future . for the NHS.’
