MSNBC doctor claims systemic factors like racism determine 80% of a person’s health while people themselves are only ‘about 20%’ responsible
A guest doctor on MSNBC claimed that people are only 20 percent capable of protecting their own health and that racism is to blame for the remaining 80 percent.
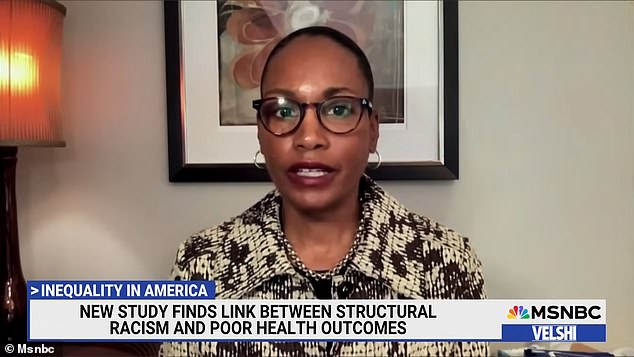
Charles Coleman Jr., who signed on for Ali Velshi on MSNBC on Saturday, brought Dr. Uche Blackstock and Dr. L. Ebony Boulware joins the show to discuss Boulware's recently published research on racism and health issues.
Blackstock, who will release a memoir next month titled Legacy: A Black Physician Reckons with Racism in Medicine, commented on how structural racism affects health outcomes.
'Individuals are only responsible for about 20% of what makes them healthy. The other 80% are these systemic factors that Dr. Boulware and her colleagues have studied in this very important research,” Blackstock said.
'I think we so often think of health as individual choices that patients make. And instead, we must truly understand how practices and policies, the legacy of slavery, the legacy of Jim Crow, and today's systemic racism, impact the health of our communities.”
Dr. Uché Blackstock (pictured) appeared on MSNBC and said, “Individuals are only responsible for about 20% of what makes them healthy. The other 80% are these system factors'
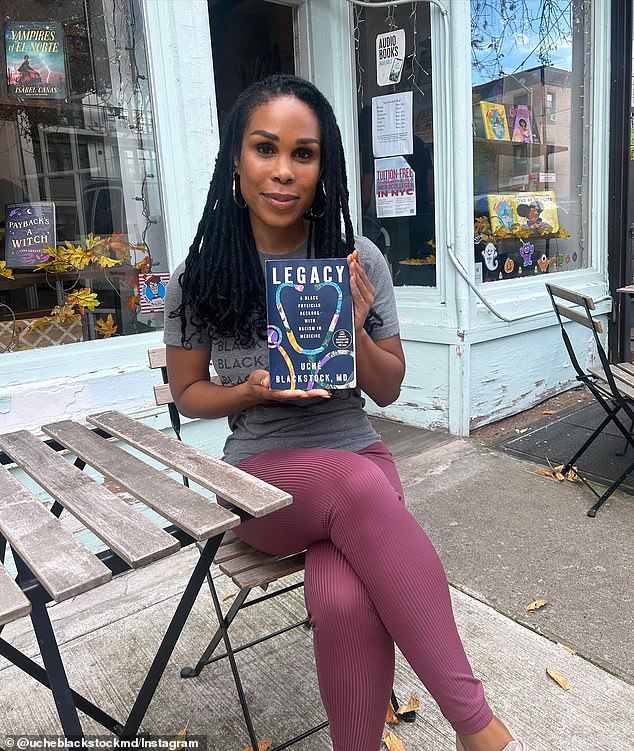
Dr. L. Ebony Boulware (pictured) recently published a first-of-its-kind study looking at how structural racism is linked to poor health
Blackstock said, “Because of discriminatory housing policies and other racist practices, we are seeing what we are seeing now in terms of these high burdens of chronic disease in our communities. Diabetes, high blood pressure, chronic kidney disease, it's basically killing us.”
Boulware's research called Residential structural racism and the prevalence of chronic health conditionspublished last week, is the first of its kind to examine how racism is linked to poor health.
The study looked at 150 neighborhoods in Durham County, North Carolina and used public data from 2012-2018 and de-identified electronic health records from 2017-2018 to examine whether structural racism is associated with higher levels of chronic health problems.
Some of the factors of structural racism that are looked at include the percentage of white residents in a neighborhood, the number of trees, crime rates, electoral participation, median income, poverty rates, unemployment and police shootings.
Boulware said, “We defined structural racism as factors that work together to create discriminatory conditions in neighborhoods that disadvantage ethical and racial minorities.”
Results showed that areas with higher structural racism indicators were associated with greater neighborhood prevalence of chronic kidney disease, diabetes and high blood pressure.

Blackstock said: 'Because of discriminatory housing policies and other racist practices, we are seeing what we are seeing now in terms of these high burdens of chronic disease in our communities'
Blackstock, who will release a memoir next month titled Legacy: A Black Physician Reckons with Racism in Medicine, commented on how structural racism affects health outcomes
“Basically what we found was that when there was more structural racism in a neighborhood, the health of the neighborhood was worse,” Boulware said.
Over the summer, the American Medical Association, the largest organization of physicians in the U.S., urged doctors to abandon body mass index (BMI) as the primary measure of healthy body weight, citing its “racist” roots of it.
The group said the metric was used for “racial exclusion” and does not take into account differences in body composition that vary based on race and gender.
The Body Mass Index (BMI), coined by a white man considering white bodies, is measured by dividing a person's weight in kilograms or pounds by the square of their height in meters or feet, and is as a way deeply entrenched in the medical system. to measure public health more broadly.
But at an individual level, BMI does not take into account relative body shape and the way fat is stored. For example, Asian people who fall within a “healthy” BMI range are still at high risk for diabetes.
