More than half of Americans with sexually transmitted diseases were infected by cheating partners, study finds
A new study finds that most Americans with a sexually transmitted disease contracted the disease from an unfaithful partner.
Fifty-five percent of people who have ever contracted a sexually transmitted disease (STD) admit that they contracted the disease because their boyfriend or girlfriend cheated on them, became infected, and then—knowingly or unknowingly—passed the disease on to others.
Nearly half of respondents had never discussed their STD status with their partner, while approximately one in eight reported that their partner had lied about their STD status.
Among people with an infection, chlamydia was the most common, followed by gonorrhea and genital herpes.
About 20 million Americans test positive for STDs each year, a horrifying statistic that experts say is evidence of a larger public health crisis, with cases of the disease reaching historic highs.
An estimated 55 percent of Americans with sexually transmitted diseases acquired them from an infidelity partner, according to a nationally representative survey.
The research, conducted by DatingNews.comsurveyed 1,000 Americans aged 18 to 79 from across the country about their sexual habits, including their practices for getting screened for STDs, and how concerned they are about contracting an infection.
Nearly one in five respondents (18 percent) indicated that they had been diagnosed with an STD.
Chlamydia was the most common infection, accounting for 36 percent of cases, followed by gonorrhea at 30 percent and genital herpes, which affected 24 percent of people.
The key to preventing infection and containing the spread is communication and honesty about one’s STI status. Hiding it from a partner increases the chance that the other person will be exposed or contract a potentially serious infection without knowing, meaning they may not know to get tested.
The survey found that more than one in three Americans have never been tested for STDs, including more than half of baby boomers (people born between 1946 and 1964) and 33 percent of millennials (born between 1981 and 1996).
Young people in their 20s tend to have the highest rates of STDs, but those rates skyrocket among older adults. Chlamydia diagnoses in people over 65 have more than tripled since 2010, while gonorrhea cases have increased about sixfold and syphilis cases have increased nearly tenfold.
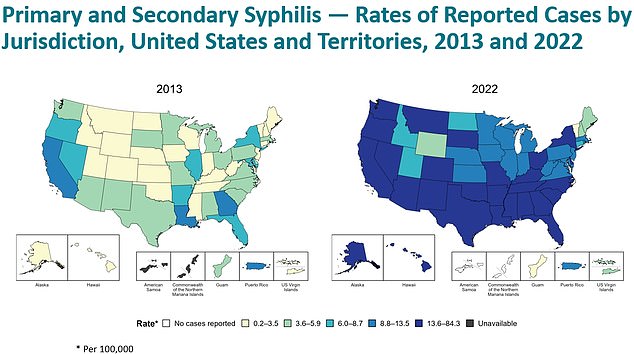
The two maps show how the number of syphilis cases in the US has changed since 2013
People who are unaware of their status often do not receive treatment in time. Furthermore, STDs that are not treated can have lifelong consequences, such as infertility, increased risk of HIV, pregnancy complications, cancer and brain damage.
Many people skip testing out of shame or fear of judgment from healthcare workers and their colleagues. Others do not get tested because they do not have access to healthcare services or because they cannot pay.
Because there is no standardized sex education in schools, many Americans don’t know the risks of disease, how to protect themselves, what signs to look for and the importance of regular screening.
Regular testing for STDs is crucial, especially for women who: often have more serious health problems due to STDs than men.
The CDC recommends annual screening of sexually active individuals, especially those under age 25 or who have new or multiple sexual partners.
In 10 to 15 percent of women with untreated chlamydia, pelvic inflammatory disease (PID) and infection of the fallopian tubes develop. This causes permanent damage to the fallopian tubes, uterus and surrounding tissue, which can lead to infertility.
The most common STD in the US is the human papillomavirus (HPV). This virus can damage the DNA in cells and disrupt the growth and death of cells. It also turns off genes that suppress the growth of cancer cells.
About 80 million Americans, or one in four, are infected with HPV, making it the most common STD in the US.
Over time, DNA damage caused by the virus changes the way cells behave, allowing them to grow into cancerous lesions that can form tumors. This can lead to cancer in a woman’s cervix.
While HPV can be prevented with a vaccine, other infections, including HIV, chlamydia, gonorrhea, syphilis, and herpes, cannot. Using condoms and getting tested regularly are the best and most effective ways to prevent infection.
Syphilis is currently skyrocketing in the U.S., after a decades-long increase that health officials say has not been brought under control since 2000.
An annual report from the Centers for Disease Control and Prevention (CDC) found that in 2022, the latest year for which data is available, there were 207,300 cases of the sexually transmitted disease (STD) diagnosed nationwide. The disorder can cause sores on the genitals and in the mouth.
That’s a 17 percent increase in one year and an 83 percent increase compared to five years ago.
The data also showed a 30 percent increase in cases of congenital syphilis, where the mother passes the disease to her baby. This is particularly worrying as it increases the risk of stillbirth and birth defects.
Experts have cited several reasons for the alarming increase, ranging from declining condom use to stigma and lack of access to preventive care to a lack of symptoms that give people a false sense of security.
About half of people with syphilis do not develop symptoms such as genital sores and rashes. They only find out they are infected when they are tested by a doctor.
Untreated syphilis can be life-threatening.
Late-stage syphilis can cause damage to the heart and blood vessels, neurological complications such as inflammation of the protective membranes covering the brain and spinal cord, blindness, and nerve damage.
Although syphilis rates have steadily increased over the past few decades, chlamydia rates appear to be generally stable.
The highest number of chlamydia cases recorded in the US since 1985 was 1.8 million in 2019. The annual average from 2020 to 2022, the most recent year for which data is available, was about 1.6 million.
Gonorrhea rates have fluctuated in recent years. The number of cases rose by 22 percent between 2018 and 2021, but fell by nine percent in 2022.
Untreated gonorrhea, like chlamydia, can lead to pelvic inflammatory disease and possibly infertility. There is also an increased risk of HIV.
And the percentages of genital herpes, mainly caused by the herpes simplex virus type 2, seem relatively flat.
Syphilis, chlamydia and gonorrhea can be cured with antibiotics. Genital herpes cannot be cured, but can be prevented by regular condom use.
