‘Mini organs’ are grown for the first time from human stem cells taken during the late stages of pregnancy – marking a ‘huge step forward’ for prenatal medicine
‘Mini organs’ have been grown for the first time from human stem cells taken during the late stages of pregnancy, marking a ‘huge step forward’ for prenatal medicine.
New research shows that complex cell models called organoids can be grown and that these ‘mini-organs’ hold the baby’s biological information.
These advances mean that human development can be observed in late pregnancy for the first time, increasing the opportunity to monitor and treat congenital conditions before birth.
Organoids – miniaturized and simplified versions of organs – allow researchers to study how organs function, both when they are healthy and when they are affected by disease.
Until now, organoids have been derived from adult stem cells or from the fetal tissue of terminated pregnancies, and regulations limit when fetal samples can be obtained.
‘Mini organs’ have been grown for the first time from human stem cells taken during the late stages of pregnancy, marking a ‘huge step forward’ for prenatal medicine. In the photo: a mini kidney
In Britain this can be done up to 22 weeks after conception, the legal limit for terminating a pregnancy, but in countries such as the US, fetal sampling is illegal.
The regulations mean that studying normal human development over the past 22 weeks has been limited, as well as for congenital diseases at a time when there may still be an opportunity to treat them.
To overcome these problems, researchers from University College London (UCL) and Great Ormond Street Hospital (GOSH) extracted stem cells that had entered the amniotic fluid, which surrounds the child in the womb and protects it during pregnancy.
Because the child is not touched during the collection process, sampling limitations can be overcome and the cells contain the same biological information as the child.
The researchers took live cells from 12 pregnancies – between the 16th week and the 34th week – as part of routine diagnostic tests.
They then identified which tissues the stem cells came from.
Stem cells from the lungs, kidneys and intestines were successfully extracted and used to grow organoids that had functional characteristics of these tissue types.
Dr. Mattia Gerli, first author of the study, said: ‘The organoids we created from amniotic fluid cells exhibit many of the functions of the tissues they represent, including gene expression and protein expression.
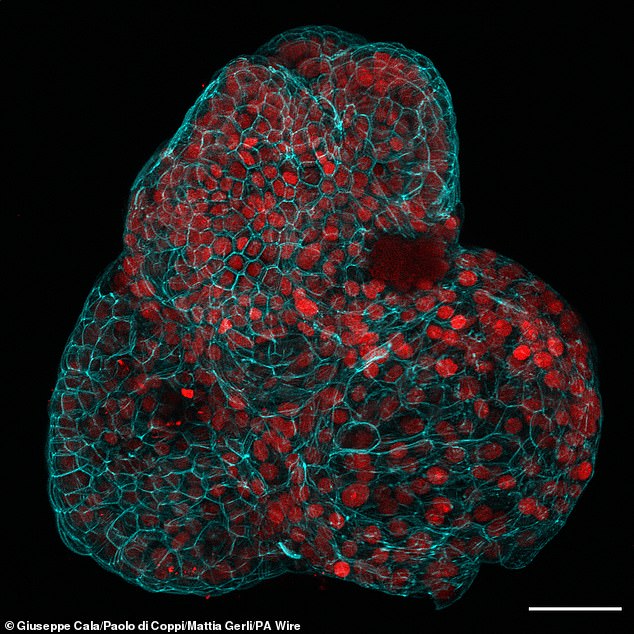
Stem cells from the lungs, kidneys and intestines were successfully extracted and used to grow organoids that had functional characteristics of these tissue types. In the photo: the mini lung
‘They will allow us to study what happens during development, both in health and disease, something that was not possible before.
‘We know so little about late human pregnancies, so it is incredibly exciting to explore new areas of prenatal medicine.’
The team worked with researchers from KU Leuven in Belgium to study the development of babies with CDH, a condition in which a hole in the diaphragm causes organs such as the intestines and liver to move to the chest, putting pressure on the lungs and hinders healthy growth.
Mini-organs from infants with CDH, both before and after treatment, were compared with organoids from healthy infants to study the biological characteristics of each group.
The study found significant developmental differences between healthy CDH organoids and pre-treatment CDH organoids.
However, the organoids in the post-treatment group looked much closer to the healthy ones, providing an estimate of the treatment’s effectiveness at the cellular level.
NIHR Professor Paolo de Coppi, senior author of the study from UCL Great Ormond Street Institute of Child Health and Great Ormond Street Hospital, said: ‘This is the first time we have been able to make a functional assessment of the innate condition of a child. before birth, which is a huge step forward for prenatal medicine.
‘The diagnosis is normally based on imaging such as ultrasound or MRI and genetic analyses.
‘When we meet families with a prenatal diagnosis, we often can’t tell them much about the outcome because every case is different.
‘We don’t claim that we can do that yet, but the ability to study functional prenatal organoids is the first step in being able to provide a more detailed prognosis and hopefully provide more effective treatments in the future.’
The researchers say that while they have not yet studied the method in relation to other conditions, it is possible that they could look at other conditions that affect the lungs, such as cystic fibrosis, kidneys and intestines.
The research was published in the journal Nature Medicine.
