Millions of obese patients taking Ozempic are at risk of gaining MORE weight – because they don’t take the drug for long enough, experts warn
There were few more words on the lips in 2023 than Ozempic, Wegovy and Mounjaro.
The blockbuster weight loss drugs – which work by suppressing hunger hormones – are highly effective.
But now experts are warning that many of the nine million prescriptions given for these drugs could be, at best, useless and, at worst, put patients at even greater risk of weight-related diseases.
That's because too many people receive courses of the drug that are far too short.
According to recent warnings, employers offer insurance plans that only cover use of the drug for a short period of time (for example, a year) to save money.
However, a growing body of evidence shows that patients who go off weekly injectable medications quickly regain the lost pounds.
At the beginning of 2022 alone, approximately 9 million prescriptions for Ozempic were written.
Additionally, stopping the medications abruptly puts patients at increased risk for weight-related health problems, including high blood pressure, elevated blood sugar levels, and changes in cholesterol.
The effects of abruptly stopping the weight-loss medications are similar to a harmful yo-yo dieting, which causes a cycle of weight loss and recovery, contributing to the risk of type 2 diabetes, heart attack and eating disorders.
Brooke Boyarsky Pratt, prescriber and CEO of the New York weight-loss clinic Knownwell, says she has had many patients tell them they would stop taking the drug after 12 months.
“I think this is going to be a compelling story given the number of patients who qualify for these drugs and the high cost of them,” she told Fierce Healthcare.
'The problem is that there is no data to support that (weight loss after one year) and in fact the data very clearly suggests the opposite.'
The problem lies with healthcare companies, which employers are increasingly turning to to secure a good insurance deal for their employees.
One of the most popular companies doing this is Calibrate, which primarily prescribes medications directly to patients.
It also partners with insurance companies to give patients the drug for about $25 a month.
More recently, it has begun to help employers negotiate better, cheaper insurance deals for workers.
As part of this, Calibrate is pitching plans that offer a limited course of medications before patients are tapered, a way to reduce costs for the employer.
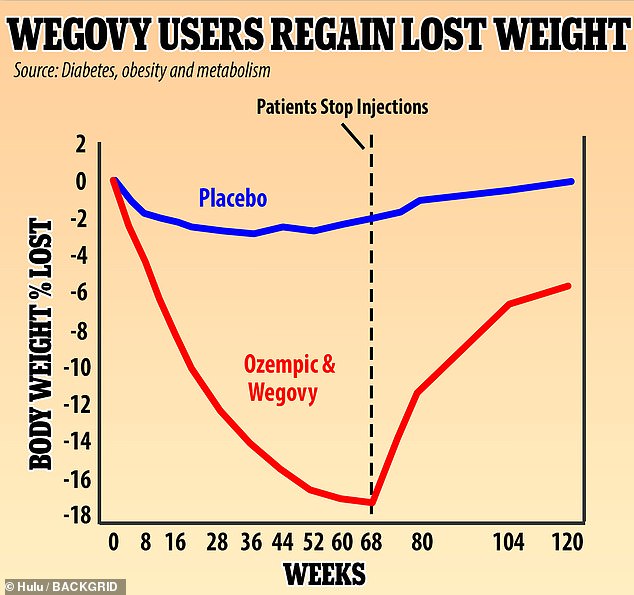
A British study found that people taking Wegovy experienced rapid weight loss, losing 18% of their weight in 68 weeks. They regained two-thirds of that weight, or 12% of their original body weight, in the year after they stopped the weekly injections. Experts say the drug must be used for a lifetime to keep the pounds off
The most recent obesity drug to hit the market was Eli Lilly's Zebpound, a rebrand of Mounjaro, the pharmaceutical giant's existing type 2 diabetes drug.
Both medications contain the active ingredient tirzepatide, which suppresses two appetite-regulating hormones, helping people feel full for longer.
Other blockbusters include Wegovy and Ozempic, the same drugs but in different doses that contain semaglutide, which promotes weight loss by mimicking the actions of GLP-1, or glucagon-like peptide-1, a hormone in the brain that regulates appetite and feelings of regulates satiety. .
Although extremely effective in helping patients lose an average of 15 to 20 percent of their body weight, the drugs cost just over $1,300 per pack, which works out to almost $270 per week or about $16,190 per year. Insurance does not always pay the bill.
Calibrate specializes in working directly with consumers who pay a one-time fee of approximately $1,700 to access one-on-one health coaching and, if eligible, a prescription for a weight-loss medication at an additional cost per dose.
The company then negotiates with insurers to give patients a monthly payment of $25 or less out of pocket. But the company has struggled to give patients timely access to the drugs amid shortages and insurers scaling back coverage.
Now Calibrate works with employers who offer health insurance to employees and with the insurance companies themselves.
The goal is to get Calibrate's program, including the drugs its doctors prescribe, covered by insurance plans that employers buy for their employees.
Companies such as Ro and Calibrate describe their weight loss programs, which include the drugs, as the most effective approach to achieving sustainable weight loss. But they fail to make it abundantly clear that most people need to continue taking the drugs to maintain their weight.
Brooke Boyarsky Pratt, founder and CEO of the well-known weight-loss clinic, said Fierce healthcare: 'I think you'll see more and more former business-to-consumer GLP-1 companies now selling to employers and claiming to have the silver bullet for GLP-1 spending.
“We're hearing from employers everywhere that this is what they're being pitched.”
Calibrate said it has designed a program to help patients taking the drugs taper their doses and eventually stop altogether, a benefit to insurers who don't have to cover the expensive drugs indefinitely.
A spokesperson for Calibrate said: 'Although the current clinical paradigm for GLP-1 treatment requires lifelong medication at the highest dose, Calibrate is investigating whether members can be taken off medication while maintaining results.
“That's why Calibrate is the first and only program with a proactive plan to get members off medication.”
Calibrate conducted its own analysis to see if its members could keep the weight off, reporting that 93 percent maintained a weight loss of more than 10 percent six to 12 months after they began tapering off GLP-1 drugs.

Influencer Remi Bader said she gained 'double the weight back' after quitting Ozempic, which she was prescribed to help deal with binge eating
The latest data showing recovery of weight loss and gains came from a study in JAMA, which showed that tirzepatide – which works like Ozempic – helped patients lose about 20 percent of their body weight after 36 weeks. But when they switched to a placebo, they regained 14 percent of their lost weight over the next 52 weeks.
The authors said: 'At least five studies (including the current study) of different classes of drugs, including powerful anti-obesity drugs such as semaglutide, have shown substantial weight regain after quitting.'
Research into the effects of stopping Wegovy and Ozempic have shown similar results. A 2022 study in the journal Diabetes, obesity and metabolism reported that patients taking semaglutide for 68 weeks lost an average of 17.3 percent of their body weight.
When they stopped treatment, they had regained 11.6 percent of their lost weight by week 120, resulting in a net weight loss of just under six percent of body weight.
Dr. Ania Jastreboff, an expert in obesity medicine at Yale University, said People: If you have a patient with high blood pressure, high blood pressure, and you give him an antihypertensive drug, and his blood pressure improves, what would happen if you stopped that drug?

Drugs like Ozempic and Wegovy are not a panacea for obesity, which experts say is a chronic disease that requires continuous drug treatment as well as healthy lifestyle habits, including exercise and a healthy diet.
'Well, their blood pressure would rise again – and that doesn't surprise us. The same goes for anti-obesity medications.”
Doctors say this is because the drugs don't treat all the underlying causes of obesity, including poor lifestyle habits and a distorted psychological relationship with food.
Dr. Elie Jarrouge, a metabolic disease expert based in Houston, said: “For people using Ozempic or Wegovy to lose weight… What is your exit strategy?
“If you don't work on changing what you eat, not just how much you eat, and your relationship with food, you will definitely gain weight again.”
Influencer Remi Bader testified to this after she gained back “double the weight” she lost while taking Ozempic.
Ms. Bader had sought treatment for her binge eating disorder, which she said became much worse when she stopped taking the drug.
She said: 'I saw a doctor and they said, it's 100% because I took Ozempic.
'It made me think that I haven't been hungry for so long, I've lost some weight. I didn't want to be obsessed with doing it for long periods of time. I was like, I bet as soon as I get out I'm going to starve again. I did, and my binging got so much worse. So then I blamed Ozempic a bit.”
