Millions of dementia patients actually have a ‘highly treatable’ liver disease that has been misdiagnosed, according to an ‘unexpected’ study
Hundreds of thousands of Americans with dementia – and millions around the world – may have a highly treatable liver disease, a study suggests.
Researchers found that 10 percent of US veterans diagnosed with dementia did not actually suffer from hepatic encephalopathy (HE) – severe liver scarring that can cause cognitive problems similar to Alzheimer’s disease.
When damage continues over an extended period of time, the liver cannot detoxify the blood, allowing toxins to build up and reach the brain.
HE can be very mild and difficult to diagnose (not all patients with cirrhosis have it, for example) and symptoms can be as subtle as changes in sleep patterns or irritability.
But once diagnosed, it can be treated with regular medications. This is usually done with laxatives that help remove ammonia and other toxins that build up in the intestines, followed by antibiotics that kill some of the harmful ammonia-producing bacteria in the intestines.
The graph above shows the number of cases of Alzheimer’s disease per 100,000 people, both age-standardized and at all ages. Age standardization is a method used to adjust for differences in age distribution between populations or over time, while non-age standardized is the raw percentage calculated for all age groups in the population without any adjustment.

A recent study of US veterans found that 10% of those diagnosed with dementia actually had a liver condition called hepatic encephalopathy (HE) – a treatable condition.
Dementia, on the other hand, is a condition caused by long-term damage to brain cells and function.
In the case of vascular dementia, this is caused by a lack of blood flow to the brain due to damage to small blood vessels from diabetes or high blood pressure.
Alzheimer’s disease, the most common form of dementia, is caused when plaques build up in the brain and cause people’s memories and other cognitive abilities to decline.
Although there are medications that somewhat slow the progression of dementia, it is incurable.
Dr. Jasmohan Bajaj, the lead author of the new study, said: ‘This unexpected link between dementia and liver health highlights the importance of screening patients for potentially treatable causes of cognitive decline.
‘Early detection of liver problems enables targeted interventions and opens up opportunities for addressing treatable factors that contribute to cognitive decline.’
More than 100 million Americans have some form of liver disease, including about 80 million people with fatty liver disease, and they don’t know it. Meanwhile, more than eight million Americans suffer from dementia.
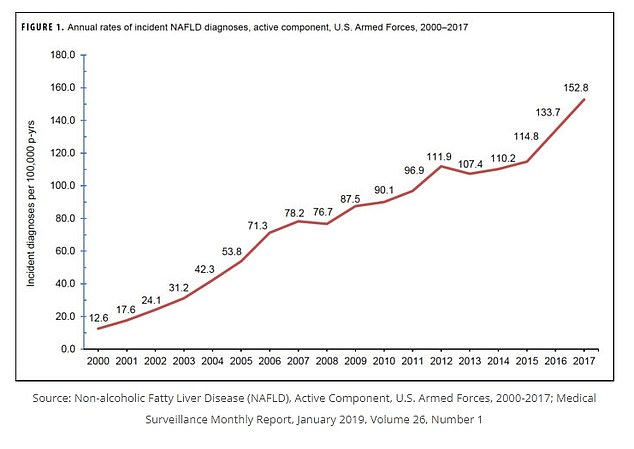
The number of cases of liver disease has increased over the past two decades, according to a study that looked at rates of the condition among military personnel.
In the new study, doctors from the Veterans Health Administration studied more than 177,000 veterans who were diagnosed with dementia during two clinic visits between 2009 and 2019. About 30 percent of them suffered from liver disease.
They looked at the group’s blood results and used them to calculate their Fibrosis-4 (FIB-4) scores, a score based on liver blood results and age, which predicts liver damage.
More than 175,000 people were involved in the analysis. Of these, 10 percent had a FIB-4 score of more than 3.25 – the cutoff value for diagnosing liver scarring.
A high score was less likely in people with diabetes, high blood pressure or kidney disease – all risk factors for dementia.
But a high FIB-4 score was more common in people with viral hepatitis and in heavy alcohol users – both major risk factors for liver disease.
This suggests that people with a high FIB-4 score may have liver disease where HE causes the symptoms rather than dementia, the authors said.
When the liver becomes scarred, it loses its ability to do its job of removing toxins that have a poisoning effect on brain cells.
When this causes HE, a patient is likely to experience a range of changes that mirror those caused by dementia, including cognitive decline and reduced motor skills, as well as poor sleep and mood.
HE occurs in the brains of about 50 percent of people with cirrhosis, which results from the toxic effect that toxins such as ammonia and manganese have on brain cells.
Deaths due to cirrhosis have increasedand the number of cases has increased over the past two decades, a study shows looked at the rates of the condition among members of the military.
At the same time, the number of cases of Alzheimer’s and other forms of dementia is increasing have steadily increased since about 2000, and are expected to continue to rise.
The study had some important caveats. Ninety-seven percent of the subjects were male, and 80 percent of them were white, even though most dementia patients are female, Hispanic or black.
It may also have been too heavy on the FIB-4 score, which does not provide conclusive evidence of liver disease.
Their research was published in the journal JAMA network opened.
The liver can be damaged in several ways, including fatty deposits, alcohol consumption and viruses. Hepatitis is the most common type of liver disease.
When the damage continues over an extended period of time, scarring can form and at some point the liver can no longer detoxify the blood. These toxins can build up and reach the brain, causing HE.
HE can be fatal, although it is treatable with laxatives to remove ammonia and other toxins that build up in the intestines, followed by an antibiotic that kills harmful bacteria.
