I’ve proven you can stop junior doctors leaving the NHS… and it’s not about money, writes PROFESSOR ROB GALLOWAY
Unless there is a dramatic change in events, next Thursday will mark the start of the eleventh round of junior doctors’ strikes.
The lack of resolution is detrimental to everyone and there seems to be no end in sight; Indeed, the determination of trainee doctors is hardening: in the latest vote, 98 percent support further strikes.
Yes, the strikes are about wages. But it is also about the circumstances. To see this, all you have to do is read the endless stories of junior doctors on their way to ‘a better life’ in Australia.
And what will not only solve the pay problems, but make a real difference, is the way in which doctors in training are scheduled.
I know this because in my hospital in Brighton the trainee doctors do not leave to move abroad, but join us.
Professor Rob Galloway (pictured) says the way to solve junior doctors’ strikes is a more flexible scheduling system

The determination of doctors in training is getting harder: in the latest vote, 98 percent support further strikes (stock photo)

Junior Doctors attend their picket line at St Thomas’ Hospital in Westminster on February 26, 2024
We don’t pay them anymore, we can’t, that’s a national decision. And it’s not about giving them special treatment instead of providing the best possible patient care.
It’s about our scheduling system. Be patient, this is not an HR lesson, but something that makes a difference for patients.
Currently, doctors in training are often only told where they will be working a few weeks before they start work. And even then, they are often treated as ‘fodder’, with endless weekends and nights, without thinking about the needs of their own lives.
This is what happened to me as a junior when I missed my best friend’s wedding. Boohoo, you might say.
But I know trainee doctors who are scheduled to work on the evening of their wedding day, or who cannot go on holiday with their children during the school holidays – instead they are told to organize their own exchanges with a colleague, if they can find it. one to do this.
This is not an urban myth, but a reality of an unacceptable way to manage staff. These highly trained doctors in training often leave medicine completely or work as doctors abroad.
The result is that the patients suffer, the doctors suffer, and billions are wasted in brokerage fees.
At my hospital, we’ve developed a new way to manage our workforce that is transformative.
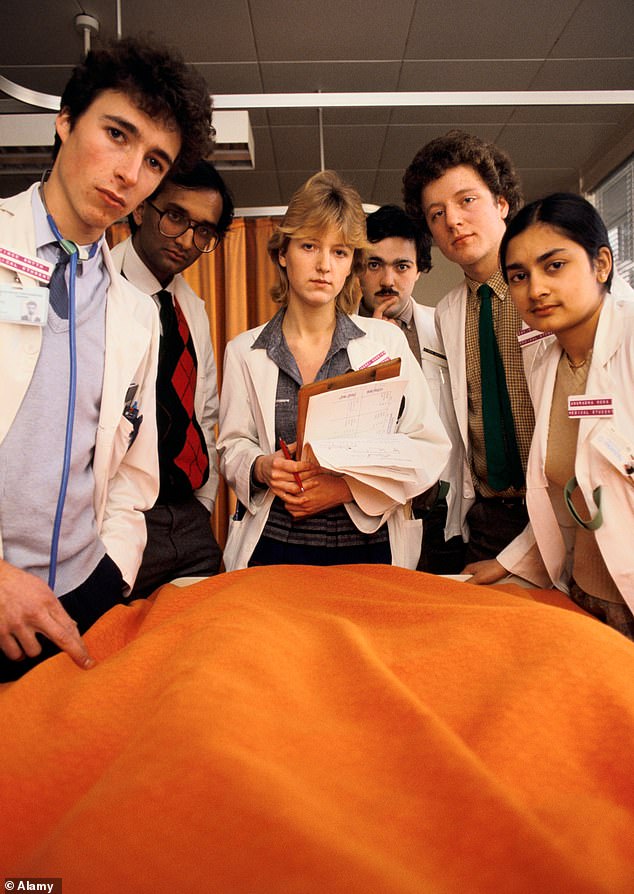
Student doctors in training tour the wards of an academic hospital

Members of the junior doctors’ committee, who are in a dispute with the government over salary arrangements, staged their tenth strike in a year on February 26
The number of hours each physician must work in each rotation (junior physicians often work in a specific area such as emergency medicine for four to twelve months before transferring to another specialty) is calculated – and then they work those hours during that rotation .
They can choose when not to work before the schedule is created.
Because the schedule is drawn up eight weeks before they start their job, it means they need to plan their leave well, but still have the work-life balance they want.
As long as we can cover the services they need, they can be free whenever they want. And if requests are submitted after the schedules have been drawn up, the roster teams are ready to help where necessary.
After we introduced this arrangement in 2016, we had one junior doctor who only worked every other weekend and occasionally full weeks due to childcare commitments.
Without our flexible scheduling she would have left the NHS. But she worked part-time for three years, knowing the hours she had committed to, before continuing her formal education. She now works as a general practitioner.
Many others – who would normally have left the NHS and worked as temporary doctors – continued to work for us on average 18 hours a week.
They can go traveling for a few months and then come back full-time for a few months, all within their contract hours.
All this is just common sense. But the main barrier to implementing these ideas has been that the standard NHS rostering system, which most hospitals use, is not designed for this degree of flexibility.
So when I managed our department schedules, I ignored the rules and worked with an independent group of computer geniuses who created a new system called healthrota.
The system, which used algorithms and sensible thinking, helped create schedules that worked for staff – and patients – and with fewer gaps in coverage, reducing expensive locum costs.

Junior doctors hold signs as they stand at a picket line outside St Thomas’ Hospital in Westminster, London, Monday, March 13, 2023

In April, NHS chief executive Amanda Pritchard wrote to hospital leaders to ‘improve rota management’.
We then rolled this out to all doctors at the trust where I work. This system has now won multiple awards, scientific papers have demonstrated its effectiveness and it has been presented by the NHS as a vanguard of good practice.
In April, the chief executive of the NHS, Amanda Pritchard, wrote to hospital leaders that they should: ‘improve rota management by exploring the opportunities offered by technology to move towards greater self-scheduling, so that doctors have more control over their lives, while meet the needs of the service”.
But the bad news is that most hospitals are not adopting this new way of working.
And the NHS team that has helped hospitals find new ways to allocate staff in recent years was disbanded last year.
Unless this is resolved, I don’t think we will resolve our junior doctor crisis, even if the pay dispute is resolved. And again, in the end, it’s the patients who will lose.
