Is US on track for an explosive outbreak in care homes this winter? CDC report shows as little as 10% of elderly residents have had their seasonal vaccines
Seniors in the US may face a “high risk of serious illness” due to their low vaccination rates. Health officials insist there is “an urgent need” to protect the vulnerable population from an outbreak of respiratory viruses.
A report from the Centers for Disease Control and Prevention today found that as of December 10, only a third of residents were up to date on their Covid vaccine and only 10 percent had received a vaccine against RSV.
A larger proportion – 72 percent – have received their flu vaccine.
Older residents in nursing homes are at increased risk of severe illness and death from one of the three viruses because of their weakened immune systems.
During the 2021-2022 flu season, the death rate among people aged 65 and over was around 7.4 per 100,000 residents, compared to 0.1 per 100,000 people in the 18 to 49 age group.
Health experts have warned that America is facing one of the worst cold winter seasons they have ever seen, as cases of Covid-19, flu and respiratory syncytial virus (RSV) continue to rise and put pressure on hospitals.
For Covid vaccines, Vermont, New Hampshire, Minnesota, Iowa, Alaska and Hawaii had the highest rates, with between 45 and 60 percent of residents vaccinated
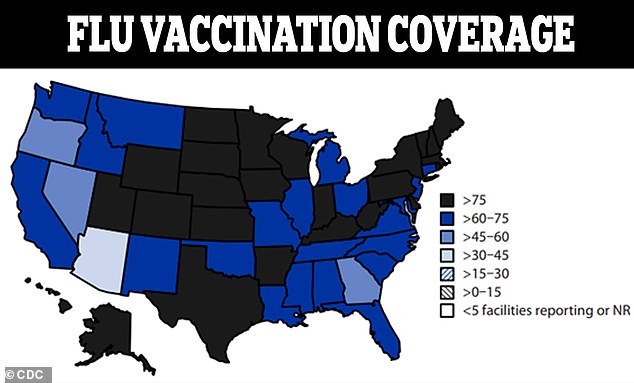
For the flu, nursing home residents with vaccination rates above 75 percent were observed in two dozen states, including Utah, Colorado, Wyoming, Nebraska, Kansas, New York, Pennsylvania and Arkansas.
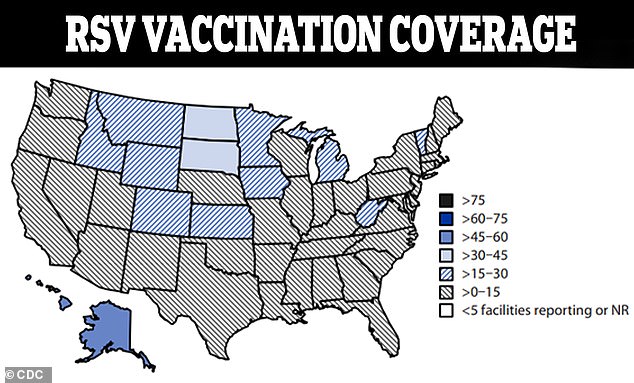
RSV coverage was the lowest, with nearly three dozen states reporting between one and 15 percent of residents vaccinated
The CDC has warned that the increase in illnesses could strain the health care system, meaning that “patients with other serious health conditions could face delays in receiving care.”
The US is already seeing a crowding of pediatric hospital beds.
The CDC said, “In some parts of the country, hospital beds for children are already nearly as full as they were this time last year.
“If these trends continue, the situation could put renewed pressure on emergency departments and hospitals by the end of this month.”
The low RSV vaccination rates may be partly due to the fact that this is the first year that the Food and Drug Administration has approved a vaccination against the virus for Americans over the age of 60.
Challenges in implementing the rollout and administration of the new vaccine, along with limited time to train providers, may also be a driving force behind low coverage.
The CDC said it will be important to educate staff and residents about RSV and the vaccine.
Overall, the health department also said vaccine fatigue, vaccine hesitancy and inaccurate health information could also lead to low numbers.
Access to vaccines in underserved areas or among vulnerable populations, as well as cost and payment barriers, also contribute.
Vaccination rates have varied across the US, with some regions having greater coverage than others.
For all vaccines, North and South Dakota consistently reported the highest coverage of all three.
For Covid vaccines, Vermont, New Hampshire, Minnesota, Iowa, Alaska and Hawaii had the highest rates, with between 45 and 60 percent of residents vaccinated.
The lowest rates – between 15 and 30 percent – were seen in 15 states, including Nevada, Arizona, Texas, Florida, Alabama and Tennessee.
Before the flu, nursing home residents with vaccination rates above 75 percent were observed in two dozen states, including Utah, Colorado, Wyoming, Nebraska, Kansas, New York, Pennsylvania and Arkansas.
The lowest rate — vaccinating between 30 and 45 percent of residents — was seen only in Arizona.
RSV coverage was the lowest, with nearly three dozen states reporting between one and 15 percent of residents vaccinated.
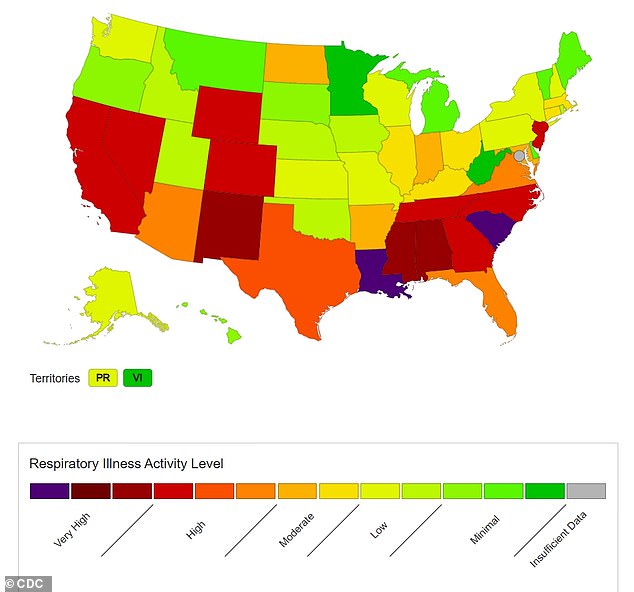
The above shows the number of respiratory illnesses in the United States as of December 9
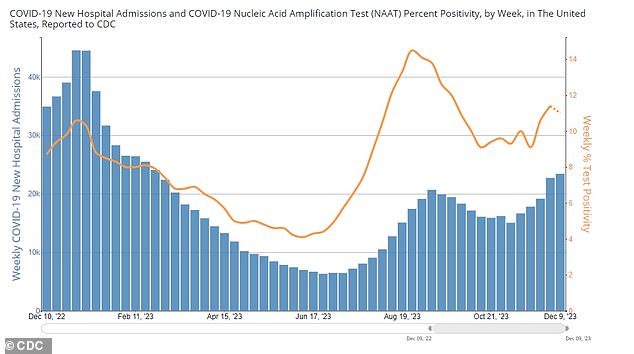
Above you can see the new weekly Covid hospital admissions (blue bars) and the weekly Covid test positivity rate (yellow line) as of December 9
States where rates were the lowest included Washington, Oregon, Oklahoma, Maine, Ohio, Mississippi, New York, New Jersey and Maryland.
Rates were highest – between 30 and 45 percent – only in Alaska and Hawaii.
The low vaccination rate is concerning as respiratory diseases have spread across the U.S. this winter.
Total respiratory illnesses have reached high or very high levels in 14 states, and hospitalizations for these illnesses have been rising for eight weeks, reaching 5.3 percent of all hospitalizations in the week ending December 9.
Covid hospital admissions have also been rising for five weeks, reaching 23,400 in the week ending December 9.
Test positivity has also increased overall over the past five weeks, reaching 11 percent in the same week.
The increase in cases is likely due to the JN.1 variant, which experts say could be more contagious.
The CDC recently announced it is monitoring the mutation and the World Health Organization announced it is considered a “variant of interest.”
The agency said it is currently the fastest-growing variant in the country and its presence will continue to increase.
The new variant was first discovered in the US in September.
Due to its rapid spread, the CDC believes it is either more transmissible or better at evading the human immune system.
Still, there is no evidence that the variant poses an increased risk to people, and there is no evidence that it is more serious than previous variants.
Additionally, experts say the current Covid vaccine offers protection.
