Infectious disease expert reveals the pathogens that could cause a new pandemic in 2025
As the country returns almost completely to normality after years of quarantine and isolation measures, the Covid pandemic increasingly feels like a distant memory for many.
But infectious disease experts are far less forgetful and have remained alert since the novel coronavirus was first identified in 2019, constantly looking for signs of mutations or other emerging threats.
Now they believe they have found one in influenza A subtype H5N1, known as ‘bird flu’, which has sickened at least 66 people in ten states. These cases resulted from people coming into contact with infected poultry and livestock or from drinking unpasteurized milk.
There has been no human-to-human transmission.
However, with each new cross-species infection, there is an increasing risk that the virus will mutate to better infect humans.
Dr. Conor Meehan, professor at Nottingham Trent University, studies how bacteria spread and evolve, with a focus on the genetic makeup of microbial communities.
He said: ‘Compared to just two cases in America in the last two years, this is a pretty big increase. Coupled with a 30 percent mortality rate from human infections, bird flu is quickly moving up the priority list of public health officials.”
This week, the US reported its first serious human case of H5N1 in Louisiana and California, where 36 of the country’s flu cases have been diagnosed, and just hours later a state of emergency was declared over the virus.
At least 66 people have been infected with bird flu. The number of cases in California has surpassed 35, prompting a statewide emergency declaration
The H5N1 bird flu does not appear to be transmitted from person to person, Dr. Meehan said, “which significantly reduces the chance of causing a pandemic in humans… in its current form, H5N1 cannot easily spread among humans.”
However, he added: ‘A recent study has shown that a single mutation in the flu genome could make H5N1 adept at spreading from person to person, potentially causing a pandemic.’
Cases of bird flu in humans have generally been relatively mild, manifesting mainly as conjunctivitis (pink eye), coughing or difficulty breathing, sore throat, muscle or body aches, diarrhea, and vomiting.
But last week, a patient from Louisiana became the first to be hospitalized with the virus. Researchers said they likely contracted the disease after handling sick and dead birds in a backyard poultry flock.
No further details are known about their symptoms, other than that they are ‘seriously ill’ with bird flu.
The CDC has not changed its overall assessment that the risk to the public from bird flu is low.
However, H5N1 has been shown to have the ability to mutate rapidly and spread between mammals.
The virus from a Michigan patient had gene segments closely related to those from dairy cows, but there were no significant changes that would improve its ability to spread between people.
Nevertheless, experts noted a mutation in that patient linked to the ability to better infect and spread mammals and increased virus replication in animals.
So while the risk of person-to-person spread remains low, if the disease is transmitted among animals, the risk of more people becoming ill increases.

The cases of bird flu in humans are due to exposure to infected livestock and poultry. The risk of human-to-human transmission remains low
Scientists at the Scripps Research Institute revealed earlier this month that just one gene mutation in the strain of bird flu virus spreading among dairy cows would allow it to attach to human cells.
The researchers changed one of the H5N1 proteins, called hemagglutinin, which attaches to human cells and allows the virus to infect.
The team generated viral proteins from the genes of the virus, taken from a person in Texas who contracted bird flu after contact with an infected cow.
They then engineered several mutations in the hemagglutinin and found that just one small change in the genetic makeup of H5N1 allowed it to switch from infecting bird cells to infecting human cells in the upper respiratory tract.
Dr. Ian Wilson, a computational biologist at Scripps and co-author of the study, said: ‘This was surprising. It was precisely this single mutation that was sufficient to change the receptor specificity.’
Governments are already showing signs of preparing for this growing threat. Britain has purchased 5 million doses of H5 vaccine that can protect against bird flu.
In June this year, Finland became the first country to offer bird flu vaccinations to people, providing two shots to 10,000 people. The vaccinations were given to workers who have been exposed to animals.
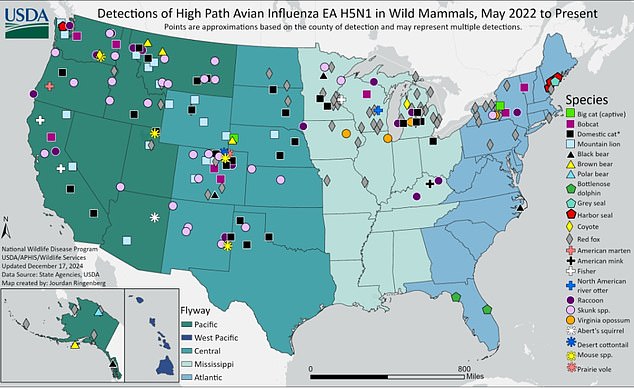
This map shows cases of the virus detected in wild mammals such as red foxes and seals
And the U.S. government has purchased vaccines and commissioned Moderna to make an mRNA bird flu vaccine
Dr. Meehan said: ‘Even without the potential ability to spread between humans, bird flu is likely to further impact animal health by 2025.
‘By understanding and preventing diseases in our environment and the animals around us, we can better prepare and combat the diseases that enter humans. Likewise, by identifying and disrupting infectious diseases in humans, we can protect our animals and the health of the environment.”
