I discovered that my baby had a tumor during pregnancy. Pioneering surgeons removed it while she was inside me
When Brailey and Louis Valenzuela learned they were expecting their second child, a girl, they were overjoyed.
They chose a name – Arley – and enjoyed an “easy pregnancy” for about six months.
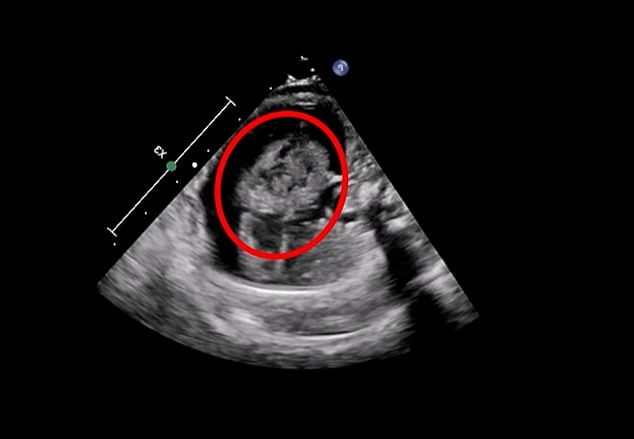
However, an ultrasound at 24 weeks revealed a potentially fatal complication: Baby Arley had an olive-sized tumor in her heart, known as pericardial teratoma.
They were told that the tumor would kill her if left untreated, growing so large that her heart would be crushed under its weight.
Delivering Arley at that moment would risk her life. At 24 weeks, her organs were still developing and her chances of surviving outside the womb were low. So the Tennessee mother was referred to a team of specialists in Pennsylvania who pioneered a procedure that allowed them to operate on the baby. while it is still inside her mother to remove the mass on her heart.
During the surgery to remove the mass, doctors cut into the mother’s stomach and partially pulled Arley out of her mother’s uterus, arms first, freeing her breast.
They always try to keep as much of the baby inside the mother as possible to maintain the protective environment that the womb provides.
While the baby was in that position, they were able to make an incision in her chest.
Arley recently visited her local cardiologist and she is doing so well that she won’t have to return for a year
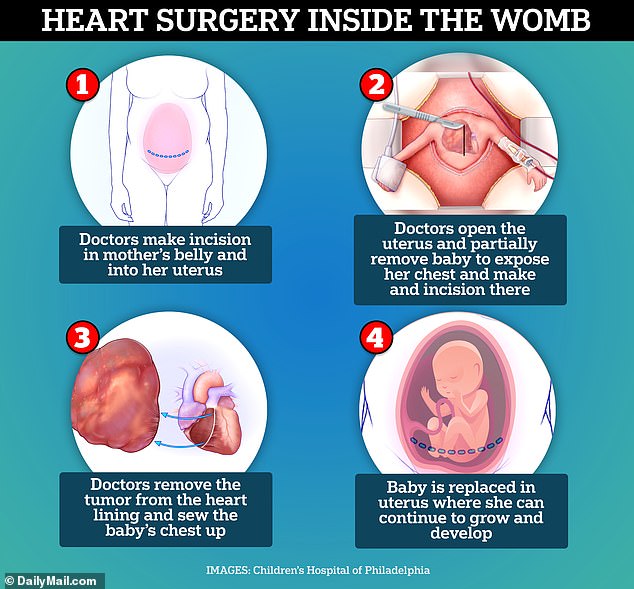
The doctors partially removed Arley from her mother’s womb by puncturing the amniotic sac, but did not deliver her completely, leaving her protected in the fluid. Specialized devices maintained amniotic fluid levels to minimize risks and prevent the uterus or placenta from reacting to the surgery
They then removed the tumor that was in the membrane surrounding the heart.
After surgery, both mother and fetus are closely monitored for signs of recovery and to detect any complications.
Mrs. Valenzuela told me Today.com that she spent about two months at Children’s Hospital of Philadelphia (CHOP), where doctors removed the tumor, until her daughter was born healthy and happy.
Pericardial teratoma in fetuses is fatal. A third of the cases result in fetal death.
The condition is rare and occurs in approximately 0.07 to 2.8 per 1,000 pregnancies. From 2000 to 2020, only 55 fetal pericardial teratomas were reported worldwide.
CHOP has performed the procedure to remove it in the womb on four babies. Exact statistics on how many are performed annually in the US are difficult to obtain.
They are so uncommon and typically performed at centers staffed by doctors with expertise in fetal surgery, it is difficult to keep track of the exact number of procedures performed each year.
All in all, the procedure took about an hour. It was a team effort, comprising specialists from cardiology, fetal surgery, maternal-fetal medicine, cardiovascular surgery, anaesthesiology, neonatology and psychology, as well as a special cohort of fetal nurses.
Brailey Valenzuela, 32, didn’t suspect anything was wrong with her pregnancy. She and her husband were excited to meet their second daughter.
But the 24 week ultrasound changed everything.
Doctors at Covenant Health’s Fort Sanders Perinatal Center in Knoxville confirmed there was a tumor in their daughter’s heart.
Ms Valenzuela said: ‘We have been told several times that the outlook is bleak and that if you don’t do something quickly – within a few days – the baby could die.’
A cardiologist in Tennessee sent Ms. Valenzuela’s medical records to the Children’s Hospital of Philadelphia, where doctors often treat complicated and life-threatening pregnancies.
“It happened so fast,” Brailey Valenzuela said.
‘They said, ‘The doctors have looked at your file and think they can help you.’ It was a huge relief.”
When they arrived in Philadelphia in December 2023, doctors had to act quickly and perform a battery of tests, including additional ultrasounds.
Within twelve hours, Ms. Valenzuela was operated on.
Dr. Jack Rychik, one of the doctors involved in Brailey Valenzuela’s surgery, said fetal tumors like this are “pretty rare.”
If left unchecked, the tumor could grow so large that it crushes Arley’s heart, which would kill her
He said: ‘It’s a tumor that grows wildly because very, very young cells… misbehave. (They) could have turned into different organs, but remain immature and decide to grow on their own.
‘The concern about the pericardial teratoma is that it grows rapidly and uncontrollably in a very confined space.’
The doctors partially removed Arley from her mother’s uterus by puncturing the amniotic sac, but never fully delivered her, meaning she was never exposed to air and was mainly protected by the fluid there. Surgeons say one of their main goals, besides removing the tumor, is to disrupt surrounding tissues as little as possible.
Doctors used specialized devices to keep the amniotic fluid level in the uterus stable, minimizing the risk of the uterus or placenta ‘feeling’ the operation.

When Brailey and Louis Valenzuela of Knoxville, Tennessee learned they were expecting their second child, a girl, they were overjoyed. But an ultrasound scan at 24 weeks revealed that their baby had a tumor the size of an olive in her heart
The body may naturally induce labor in response to disturbances, but these devices, along with anesthesia techniques, help prevent labor, labor, or changes in blood flow by ensuring that the uterus maintains its shape and fluid levels during the procedure.
Without intervening, the mass on Arley’s heart could have grown so large, perhaps two to four times larger than the heart, and pressed against it, preventing it from filling with blood.
Dr. Rychik said, “You cannot survive if the heart cannot be filled. That makes these tumors deadly.’
Arley weighed only 1.8 pounds when this happened.

Arley was born at 35 weeks, which is considered preterm. But the operation was a great success. Heart heart functioned normally

Ms. Valenzuela gave birth via caesarean section in February 2024. The doctors discovered that her uterine lining was very thin and could tear if they did not deliver Arley right away.
When they removed the tumor, surgeons saw that it was slightly attached to the aorta, the largest artery in the body that carries oxygen-rich blood from the heart to the rest of the body.
After removing the tumor and repairing the tear in the aorta, doctors stitched Arley back up, returned her to her mother’s womb, and closed Brailey’s abdomen.
When she woke up, Mrs. Valenzuela looked for her husband and sleepily pointed to her stomach as if to ask if Arley survived.
She said: ‘I remember him saying, ‘The baby’s fine. The baby is doing well.” That’s all I needed to hear… it was a huge blessing.”

Arley is healthy and happy. Her mother says her heart functions like that of other babies
Within a few days, Arley’s heart began to function normally. All the while, Ms. Valenzuela remained in Philadelphia, where she was under close supervision until the birth. When she developed severe abdominal pain on February 17, 2024, doctors discovered that her uterine lining was very thin.
To avoid a rupture, they delivered Arley via C-section at 35 weeks, which is considered preterm.
Ms Valenzuela said: “Her heart was amazing. It functions just like any other baby.”
Arley recently visited her local cardiologist and she is doing so well that she won’t have to return for a year.
“She’s doing great,” Ms. Valenzuela said.
“I hope people can have hope when they read Arley’s story.”
