How It Took Olivia Munn THREE TIMES to Get the Correct Cancer Diagnosis — After Mammograms and Genetic Tests Were Negative… and the Doctor Who Finally Got It Right
Olivia Munn has credited her doctor with ‘saving her life’ after spotting her breast cancer – which was missed by a genetic test and mammogram.
The actress, 43, revealed on Wednesday that she was diagnosed with the disease just two months after being given the all-clear from a mammogram and do-it-yourself genetic tests, which claimed to detect 90 genes linked with cancer.
However, when her obstetrician calculated her disease risk, based in part on her family history of the disease, she feared that Munn had a one-in-three chance of developing the disease and sent her for further evaluation.
That led to Munn being diagnosed with luminal B breast cancer in both breasts at an early stage. She then had a double mastectomy to prevent the cancer from spreading to other parts of the body when it became fatal.
Doctors told DailyMail.com that although mammograms are considered the gold standard for detecting breast cancer, the scans can still miss as many as one in eight cases due to several factors, including how small the tumors are and how dense the breasts are. be the woman.
Dr. Christoph Lee, a professor of radiology who specializes in breast cancer screening at the University of Washington, told DailyMail.com that “missing tumors on mammograms are not uncommon.”
Olivia Munn has revealed she was diagnosed with luminal B breast cancer last year after undergoing four operations in the past ten months. She credited her OBGYN (here) with ‘saving my life’
Munn initially had a mammogram, which came back negative two months before her cancer diagnosis
In addition, up to 70 percent of tumors can go unnoticed if a woman has particularly dense breasts, making it difficult to detect masses on the X-ray scans.
Experts also said that at-home genetic tests such as 23andMe and Ancestry, aimed at finding genes linked to cancer, should not be intended to test for cancer themselves.
Munn revealed that she took a commercial genetic test in February 2023 that could reportedly detect 90 genes linked to cancer.
She claimed hers was negative for all genes, including BRCA, which has the strongest link to breast cancer and is also called the Angelina Jolie gene.
She also had a mammogram that winter, which was negative. It’s unclear whether Munn was experiencing symptoms or only undergoing routine screening every two years, which health officials recommend women start at age 40.
“Two months later I was diagnosed with breast cancer,” she said on Instagram.
Despite the negative test, Munn’s gynecologist decided to calculate her breast cancer risk assessment score.
The doctor determined that based on her age, family history and the fact that she had her first child after age 40, the actress had a 37 percent risk of developing the disease.
“The fact that she did that saved my life,” Munn said.
Based on that score, Munn was then referred for a breast MRI and ultrasound, which revealed luminal B cancer in both breasts. Just 30 days later she had them removed.
Breast cancer is the most common form of cancer in both the US and the world.
The National Cancer Institute (NCI) estimates there will be more than 300,000 new cases this year, along with 43,700 deaths.
Mortality rates fell by 43 percent between 1989 and 2020, following successful public health awareness campaigns, better screening and new medications.
And nine out of ten patients are expected to survive after five years.
Luminal B breast cancer starts in the inner (luminal) lining of the breast ducts, which are thin tubes in the breast that transport milk from the breast to the nipple.
This form of the disease accounts for about 10 to 20 percent of breast cancer cases and is considered more aggressive than other forms.
According to the Susan G Komen Foundation, women with luminal B tumors are often diagnosed at a younger age.
More than 98 percent of those whose tumor was diagnosed locally – before it spread – are expected to survive after four years. Once the cancer spreads to other areas, that rate drops to 46 percent.
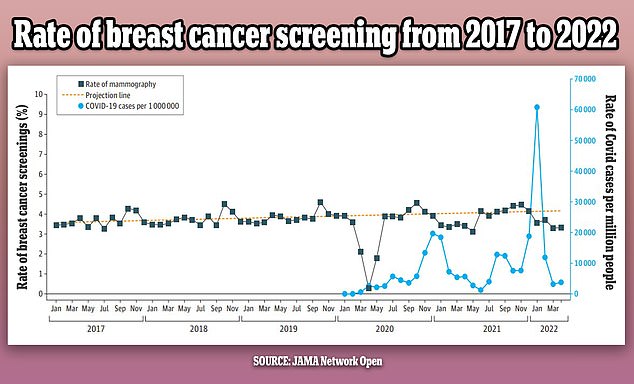
The graph above shows the changes in breast cancer screenings (black line) per month since 2017. It also shows a predicted screening rate (yellow dotted line) and Covid infection rate (blue line) in the US over the same period. The number of screenings was initially stable, but fell by as much as 14 percent in the first year of the pandemic

A mammogram is a type of X-ray in which the breasts are placed between metal plates to flatten them and get images from above and from the sides
A mammogram is considered the ‘gold standard’ for diagnosing breast cancer.
This is a type of X-ray in which the breasts are placed between metal plates to flatten them and get images from above and from the sides.
Currently, all women over 40 are advised to have a mammogram every two years.
However, the test is not always completely accurate. In fact, the American Cancer Society (ACS) estimates that mammograms miss one in eight cancers.
“Mammography is the standard of care for breast cancer screening, and it is actually a very sensitive test,” Dr. Lee said.
“The sensitivity in the United States is about 87 percent, which means that if breast cancer is present, a radiologist can detect it 87 percent of the time.”
However, the test cannot detect everything. In fact, the American Cancer Society (ACS) estimates that mammograms miss one in eight cancers.
Dr. Melissa Durand, a radiologist specializing in breast imaging at the Yale School of Medicine, said in a university blog post: ‘With conventional mammography we can be up to 98% accurate in a fatty breast, but in women with extremely dense breasts our sensitivity can drop to only 30%.’
Breasts are made up of fatty, glandular, and connective tissue, and breast density is a measure of how much dense tissue (glandular and connective tissue) there is compared to less dense (fat).
Breasts are classified into four categories: A, B, C and D.

Several at-home genetic tests claim to detect cancer genes from spit and urine samples. However, doctors warn that they cannot predict the risk of cancer

Olivia, mother of two-year-old son Malcolm Hiệp (pictured), said she had both breasts removed 30 days after her diagnosis
Those in the A group have almost entirely fatty tissue, while B has scattered areas of dense tissue.
C breasts contain denser than fatty tissue, and D are considered ‘extremely dense’.
According to the NCI, about 50 percent of American women have dense breasts. Breast density is often hereditary, although having a low body mass index (BMI) or taking menopausal hormone medications can increase density.
However, growing older and having children can lead to fatter breasts. Dr. Lee noted that breast density is measured during a woman’s first mammogram, so she wouldn’t know if she has it until she undergoes a test.
“Women with dense breasts have a higher risk of breast cancer than women with fatty breasts,” the NCI states. “This risk is separate from the effect of dense breasts on the ability to read a mammogram.”
It is unclear whether Munn’s cancer was missed due to dense breasts or some other factor.
“Unfortunately, about 13 percent of mammograms are occult, meaning they are not visible on the X-rays of an MRI,” Dr. Lee said.
These are usually smaller tumors, but also tumors that are masked by dense breasts.
Munn also said that prior to her mammogram, she used an at-home genetic test that claims to detect up to 90 cancer genes.
23andMe and Ancestry are two of the most popular, although it is unclear whether she used one of these or another method.
Dr. However, Lee cautioned against using any of these tests as the sole method of determining your risk for breast cancer, whether you are positive for these genes or not.
‘A genetic test does not tell you exactly what your risk of breast cancer is. Only a very small proportion of breast cancers are due to genetic mutations such as braca one or bracket two,” he said.
‘The vast majority of breast cancer cases are found in women with no family history of breast cancer, and no genetic mutations.’
If you are experiencing symptoms of breast cancer — such as a lump, change in breast shape, flaky skin around the nipple, and inverted nipple — and have a negative mammogram, Dr. Lee recommends having a diagnostic mammogram or breast ultrasound.
Diagnostic mammograms are typically performed on women with symptoms of breast cancer and may include additional images that are not part of screening mammograms.
An ultrasound uses sound waves to show breast changes and cysts.
He also noted that people with a primary family history of the disease, such as a mother or sister, should get an MRI along with symptoms.
‘It is important to assess your breast cancer risk with your midwife or a GP,’ he said.
