Has dementia plateaued in the US? Mysterious CDC data cast doubt on predictions of spiralling diagnoses
The number of dementia cases in the US appears to have reached a plateau, casting doubt on previous predictions of an upward trend in diagnoses in the coming years.
The CDC’s latest National Health Interview Survey reported that four percent of American seniors over the age of 65 have dementia, a figure that has remained largely unchanged since the last poll in 2019.
This figure is lower than the number of seniors with other chronic conditions, such as heart disease, which affects 14 percent of people between the ages of 65 and 74, and cancer, which occurs in the lives of 17 percent of the age group.
The data shows that previous dire predictions that the number of diagnoses will reach 14 million by 2060 – driven in part by the US’s increasingly aging population – may be an overestimate.
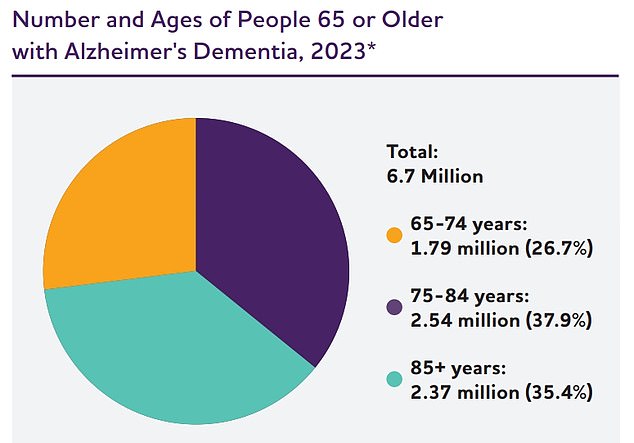
The above pie chart was created based on data from Rajan et al. Due to rounding, percentages do not add up 100
The questionnaire more than 9,200 people aged 65 and over were contacted and asked by telephone or in person whether they had ever been diagnosed with dementia, including the most common form, Alzheimer’s disease.
The CDC researchers interviewed people from all walks of life, taking into account race, education level, household income as a percentage of the federal poverty level, where they lived and whether they were veterans.
Overall, the researchers found no statistically significant difference in dementia rates between 2019 and 2022.
Have diagnoses steadily increased over the past fifteen years, from 4.7 million seniors with the disease in 2010 to 5.8 million in 2020, according to a 2020 report from the Alzheimer’s Association.
However, a number of other studies seem to suggest otherwise.
A study published in the journal Neurology contained data from nearly 50,000 participants who were followed for 27 years between 1994 and 2000.
They found one The total risk of dementia has decreased by an average of 13 percent since 1998.
Meanwhile, the Population Survey Bureau reported that a smaller percentage of the total elderly population is diagnosed with dementia every year.
Improvements in healthcare, better management of lifestyle-related risk factors and increased awareness may contribute to this decline.
A growing number of people embracing healthy lifestyles, especially heart-healthy behaviors, could help lower rates.
Dr. Keith Vossel, Alzheimer’s program director at the department of neurology at the University of California, Los Angeles, told DailyMail.com: ‘Dementia rates are stagnating in the US, likely due to better attention to modifiable risk factors such as high blood pressure and overall condition.
‘The number of cases of dementia continues to rise in developing countries.’
However, other researchers told DailyMail.com that some data showing a plateau – for example the new CDC numbers – are based on unreliable studies.
Dr. Elizabeth Landsverk, a geriatrician based in New York, told DailyMail.com that the survey left out some crucial questions, potentially excluding a large portion of people.
She said, “They’re talking about non-institutionalized older adults with a diagnosis of dementia. Many people with the condition are in full-time care and would be missed in the research.’
Other experts have highlighted that the pandemic, which occurred between the two trials, may have meant that fewer people were able to access screening and receive a diagnosis.
Dr. Landsverk said: ‘TThere are several hurdles you have to overcome to be able to say that someone has been diagnosed.”
The CDC’s data collection could also have been unreliable because it relied on patient answers — and people with dementia may have difficulty answering questions accurately.
An estimated seven million Americans suffer from dementia, with Alzheimer’s disease being the most common form.
The degenerative condition is associated with aging and causes parts of the brain involved in memory consolidation and formation to atrophy.
Concerns about the rise in dementia cases have centered around the rise of the elderly population in the US, with the number of Americans over the age of 65 increasing more than tenfold over the past century, to 55.8 million.
This number is expected to reach 82 million by 2050, with the demographic share of the total population growing from 17 percent to 23 percent.
Experts predict that the aging population, along with unhealthy lifestyle habits, will likely lead to a rise in dementia cases in the coming decades.
It is also likely that Covid itself, which has been shown to damage blood vessels and cause lifelong vascular problems, will cause more cases of dementia.
There is currently no cure for Alzheimer’s disease and few treatments are available. But there is hope for more.
The FDA’s committee of independent advisors voted unanimously this week to recommend approval of Eli Lilly’s drug donanemab.
The monoclonal antibody slowed cognitive decline in patients suffering from the early stages of the disease. It carried the risk of swelling and bleeding of the brain, but the committee ruled that the consequences of Alzheimer’s disease are so serious that any benefit is worth it.
The drug is based on a long-standing belief that Alzheimer’s disease is rooted in dysfunctional cell activity in the brain that causes the buildup of a protein called amyloid beta. When these proteins accumulate, they form clumps that cause a domino effect that results in the death of brain cells.
Another amyloid-fighting drug was recently approved. Leqembi was approved last year and while it also showed modest benefit, it was thought to have benefits that outweighed the risk of brain bleeding.
