FDA sued for failing to act on claims that SSRI antidepressants can kill sex drive and shrink genitals even AFTER discontinuing use
The FDA is being sued for allegedly ignoring evidence that antidepressants permanently ruin patients’ sex lives — even years after they stop taking the drugs.
Selective serotonin reuptake inhibitors (SSRIs) like Prozac and Zoloft were only labeled with a warning that users could cause erectile dysfunction, low libido, vaginal dryness and difficulty ejaculating after patients began complaining to their doctors about sexual side effects in the 1980s and 1990s .
But thousands of former patients say they are completely asexual, numb below the waist, and unable to enjoy sex or maintain romantic relationships. Some patients have even experienced shrinkage of their genitals.
The FDA is now being sued by a team of scientists who say the FDA ignored this their petition has been calling for a warning about permanent sexual side effects since 2018, asking the agency to warn doctors and patients about the long-term risks.
The condition mentioned in the lawsuit is post-SSRI sexual dysfunction (PSSD), which can cause genital numbness, a complete loss of libido, erectile dysfunction and other sexual function problems for years after the drugs are stopped.
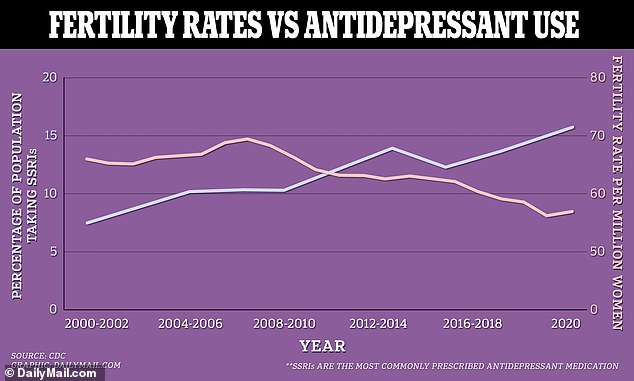
As the fertility rate in the US gradually declines, more and more Americans are being prescribed SSRIs, the most common type of antidepressant. These medications can lead to lower sperm quality in men
An estimated one in ten Americans aged twelve and older uses an antidepressant.
The lawsuit was filed by Dr. Antonei B. Csoka, a molecular biologist at Howard University,
The specific condition Dr. Csoka refers to in his complaint is post-SSRI sexual dysfunction (PSSD), which can also cause genital numbness, premature ejaculation, and emotional blunting.
The agency said in 2018 that it would further review the science and contact him, but that never happened.
The FDA’s alleged lack of follow-up contradicted its own protocol, which states that citizen petitions must be responded to within 180 days.
Although the FDA has failed to add the proposed warning label, regulators in Europe and Canada have already done so.
Scientists aren’t sure how many people are affected by PSSD, although it is more half of all antidepressant users have reported some degree of sexual dysfunction while taking it.
A 2018 review of the scientific literature on PSSD found that about five to fifteen percent of people taking antidepressants developed sexual side effects such as erectile dysfunction and lack of sex drive after taking SSRIs and SNRIs.
Dr. Csoka is an advisor to the PSSD Network, an advocacy organization that encourages patients to tell their stories to raise awareness and hopefully find a cure for long-term sexual dysfunction.
Commonly prescribed antidepressants include SSRIs, which increase levels of mood-regulating serotonin in the brain, and SNRIs, which increase levels of both serotonin and another neurotransmitter, norepinephrine, currently include package labels warning of sexual side effects.
Drug manufacturers are required to warn patients and prescribers that their medications can cause low libido and a decreased ability to orgasm, but they are not required to disclose that these effects may be permanent.
Dr. Csoka said: ‘Without adequate warnings about the risk of possible permanent damage to sexual function, patients and healthcare professionals cannot weigh the benefits of using the drugs against the possible harms.’
Patients who shared their stories through the PSSD Network have described a range of disorders ranging from erectile dysfunction, genital shrinkage and numbness to a lack of any sense of attraction to others and an inability to feel pleasure.
One male patient had been prescribed several antidepressants at age 16 to cope with the death of his father, and was able to stop taking them at age 20.
Now, at age 25 and off medication, he has ‘extreme genital shrinkage and discomfort, I have neurological dysfunction of the smooth muscle in my penis, which causes hypercontraction or persistent arousal disorder.
“I have an overactive bladder all the time, I have to urinate, I have severe erectile dysfunction and premature ejaculation… I never had this before the meds.”
He added: ‘I have seen a urologist who specializes in sexual health acknowledge the existence of PSSD; he did an ultrasound of my genitals and told me I have fibrosis, and he said it’s very common to see that in men who have been on antidepressants for a while.”
Meanwhile, a female patient stopped taking her antidepressant three years ago but now told her sexuality has disappeared.
She said, “My clitoris feels like a dead lump.”
And a third patient who took Lexapro for about three months said he “now asexual of the medicine.’
He said: ‘I used to be able to look at people I was attracted to and feel something, but now I don’t feel anything, it’s like looking at the wall. By essentially taking away almost all the positive emotions, they went from a hundred to maybe less than one, it’s that strong.”
He added that the hardest part is the general emotional numbing caused by the drugs: “When you hug the people you love, your mother, your father, your nephew, you don’t feel anything… You can’t have any emotional connection at all. ‘
Dr. Csoka has been researching antidepressant-related sexual dysfunction since the early 2000s and was among the first to propose that the drugs, as a side effect of increasing serotonin levels in the brain, caused DNA modifications that affect activity of genes that regulate blood pressure. sexual function.
He told the Guardian: ‘Several scientists, including myself, have published studies showing that an SSRI can alter epigenetics and human cells.
‘If that happens, those cells or tissues may not immediately return to how they were once treatment stops. It’s like an imprint has been left behind. However, it is still not known exactly what these epigenetic changes are. So what we need to do is limit it – what’s happening?’
His lawsuit archived in the US District Court for the District of Columbia is seeking to force the FDA to rule on the petition.
In America, fertility rates have fallen to historic lows in recent years, due to a large population of women who want to focus on their careers before starting a family, and a sedentary lifestyle that reduces fertility.
But an explosion in antidepressant prescriptions over the past two decades is also blamed for the country’s baby bust.
A 2022 meta-analysis in Frontiers in pharmacology found that SSRIs “have a statistically significant impairment of semen quality, such as sperm concentration, sperm morphology, and sperm motility,” the researchers wrote. However, semen volume was not affected.
Since becoming widespread in the 1980s, prescriptions for the mood-boosting drugs have soared, with a record of nearly one in five adults taking them in 2020, compared to about one in fifty at the turn of the century.
This could contribute to the overall fertility rate in the US, which has been steadily declining for decades.
According to the United Nations World Population Prospects, women had an average of just 1.7 children in 2020. In 1970 that percentage was 2.3.
The global fertility rate – the average number of children each woman has – was 2.3 in 2020, compared to 4.7 in 1970. This is a staggering drop of 51 percent.
