FDA authorizes first at-home test for chlamydia and gonorrhea as cases of STDs skyrocket across the US
The Food and Drug Administration has authorized the first-ever home diagnostic tests for chlamydia and gonorrhea in hopes of controlling America’s STD epidemic.
Instead of requiring people to travel, the newly authorized test kit is administered after a health questionnaire is completed by the patient and reviewed by a doctor.
It is then sent directly to the patient for home use, before being returned by post to a laboratory for analysis.
The Simple 2 Test will be marketed by LetsGetChecked, a New York-based company specializing in laboratory testing where people take samples in the comfort of their own home and send them to a laboratory, which returns the results securely online.
The new test does not require a prescription and will save people a trip to a doctor’s office for invasive testing and help people seek treatment before their infection worsens.
Federal regulators celebrated this as a public health victory that will help combat the steadily rising number of STDs in the U.S., a worrying trend that worsened during the pandemic as access to regular preventive care was hampered.
Gonorrhea has been on the rise since 2012, with rates per 100,000 in men significantly higher than in women
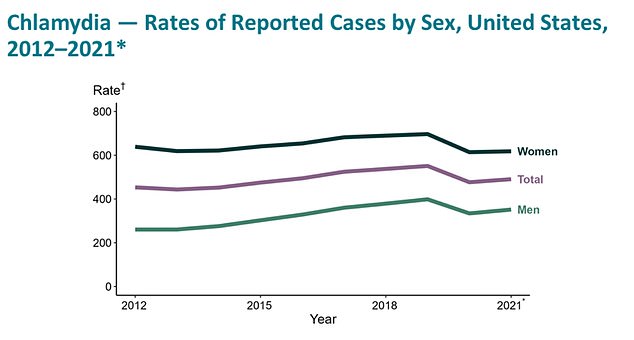
Chlamydia has been on a steady increase since 2012. But since 2001, cases have more than doubled
Dr. Jeff Shuren, director of the FDA’s Center for Devices and Radiological Health said Thursday: “This authorization marks an important public health milestone, allowing patients to learn more about their health from the privacy of their own home.
“We are eager to continue supporting greater consumer access to diagnostic testing, which will help our goal of bringing more health care into the home.”
After HIV, which can be screened at home with an antibody test, this is the first FDA-approved self-test.
For $99, the Simple 2 test is sent to someone’s home in discreet packaging. After receiving the kit, patients must complete a health questionnaire for a doctor to review. They will then collect and submit vaginal swabs or urine samples, which can detect the bacteria that cause gonorrhea and chlamydia.
Users then mail their kits for free to the same accredited labs used by doctors’ offices and hospitals, which the company says ensures accuracy.
People receive their results within two to five days via a secure online portal. If the test is positive, they can consult a healthcare provider to discuss treatment options.
The biggest risk with using the at-home test is receiving a false negative result, which can “result in delays in effective treatment, progression to disseminated disease, and spread of infection to other individuals in your community,” the FDA said.
The company can also help administer necessary medications to the patient if they consult a doctor after a positive result.

Less than half of men use condoms, compared to between 75 and 55 percent since 2011, and an increasing number rely on women to use contraception
The company said its services will also benefit the partners of those who test positive: “If your results are positive and you qualify for treatment, we can also offer treatment for your partner(s) at an additional cost. All they have to do is start their own virtual consultation and we can help them on the same path to peace of mind.”
Low access to preventive care and disease screening during the pandemic, in addition to lax attitudes towards contraception, were the main causes of the increase in STD cases.
According to the Centers for Disease Control and Prevention (CDC), there were 2.53 million cases of chlamydia, gonorrhea and syphilis in 2021, up nearly 6 percent from 2020 and up 7 percent from 2017.
Moreover, the increase can also be attributed to the fact that less than half of men use condoms, up from between 75 and 55 percent since 2011. An increasing number now rely on women to use contraception to prevent pregnancy.
However, contraception does not protect against STDs, according to an annual report on family planning from the Bureau of Population Affairs.
Between 2020 and 2021, the rate of gonorrhea among men increased by more than six percent (from 234.8 to 249.7 per 100,000 men) and among women by more than two percent (from 173.8 to 177.9 per 100,000 women).
Chlamydia cases, which had become more common at 1.58 million cases in 2020, skyrocketed to 1.64 million in 2021.
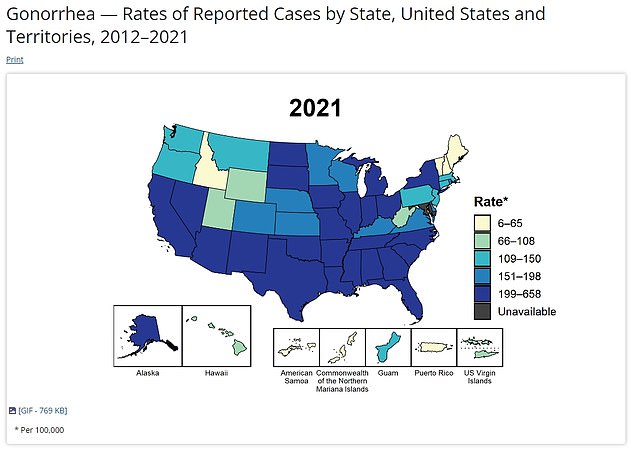
The above map shows cases of gonorrhea in the US in 2021
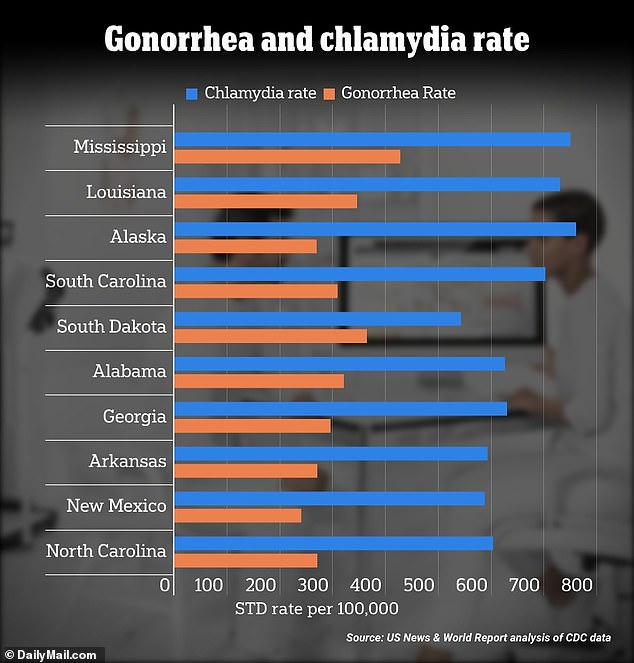
Alaska, a largely rural state where access to health care may be limited, had the highest rate of Chlamydia. It has a relatively young population, which is generally more likely to contract STDs
Dr. Leandro Mena, director of the CDC’s STD Prevention Division, issued a stark warning last spring that the STD epidemic in the US “shows no signs of slowing.”
New data published in the New England Journal of Medicine As for doxycycline, one of the most commonly used STD drugs, which is cheap and has been sold for half a century, it gives doctors some hope that the STD epidemic can be contained.
The study, published in April, looked at 501 gay men, bisexual men and transgender women in Seattle and San Francisco with a history of sexually transmitted infections who had taken one doxycycline pill within 72 hours of unprotected sex.
Participants who took the pill were about 90 percent less likely to get chlamydia, 80 percent less likely to get syphilis and more than 50 percent less likely to get gonorrhea compared to people who didn’t take the pills after sex.
Whether the CDC will formally recommend doxycycline as another type of morning-after pill is still in question, as officials must consider many factors, such as the drug’s adverse health risks.
For example, when combined with the blood thinner warfarin to treat or prevent blood clots, doxycycline can further thin the blood, increasing the risk of serious bleeding and bruising.
Other medications, including over-the-counter antacids and some barbiturates, make the medication less effective.
A recent analysis conducted by the health research firm InnerBody used federal data to rank the cities with the highest rates of STDs, including HIV, chlamydia, gonorrhea and syphilis.
Southern cities were disproportionately represented in the roundup, which looked at metropolitan areas in the US.
They accounted for 14 of the top 25 states with the highest concentrations of STD cases.
And most of the top-scoring cities were in states that spend less than the national average on health care for their citizens.
