Doctors warn that common reflux drugs could cause scurvy – after the Victorian disease struck a 50-year-old man
You might assume that scurvy is a disease that became extinct in Victorian times.
But according to recent reports, the condition is making a comeback, with cases increasing by 25 percent since 2007. This is believed to be due to the increased reliance on junk food during the cost of living crisis.
Now experts have warned that it is not just malnutrition that is causing the rise in the disease, which causes red spots on the skin and can be fatal if left untreated.
A common reflux drug taken by millions of Britons can also cause scurvy, according to a recent report.
Writing in the British Medical Journal Case Reports, doctors at Sir Charles Gairdner Hospital in Western Australia warned that proton pump inhibitors (PPIs), such as omeprazole, could be a culprit.
This is because these medications reduce the production of acid in the stomach, making it harder for your body to absorb vitamin C.
In July, doctors reported the case of a man in his 50s who developed the condition after taking PPIs and following a diet lacking vitamin C – which is essential to prevent the disease.
The first sign of the disease was a reddish-brown rash that covered the man’s legs and spread to his hands and arms.
Doctors in Australia described a man in his early 50s who showed signs of scurvy in a study published in BMJ Case Reports. The image shows the progression of his rash to his upper extremities

The man, who recently underwent bariatric weight loss surgery, had a reddish-brown rash that covered his legs (pictured) and spread to his hands and arms

The study notes that taking medications that interfere with vitamin C absorption, such as proton pump inhibitors, which treat acid reflux, can also cause the condition.
The case study describes how doctors performed blood tests that ultimately showed he had no vitamin C in his bloodstream. He also had very low levels of other important nutrients – another sign of scurvy.
He was given daily vitamin C (1000 mg), vitamin D3, folic acid and multivitamin supplements, which cleared up his painful rash. Vitamin C levels quickly returned to normal.
Doctors discovered that in addition to taking PPIs, he had not been eating fruits and vegetables and had even been skipping meals.
It was also revealed that he had done so recently underwent bariatric treatment weight loss surgery and could not afford to continue purchasing the nutritional supplements he had been prescribed.
Weight loss surgery – which makes the stomach smaller so it feels full more quickly – can make it harder for your intestines to absorb vitamins and minerals from food, putting you at risk of malnutrition, the NHS warns.
But patients are usually put on a strict diet and given vitamin and mineral supplements to prevent this.
The report highlights several risk factors for scurvy in modern times, such as lack of access to good quality nutritious food, eating disorders, low household income, obesity, alcoholism, smoking and kidney dialysis.
The case study authors wrote: ‘Our patient had multiple risk factors, namely poor dietary habits, obesity, previous bariatric surgery, use of proton pump inhibitors and low income. His history of iron, vitamin D and folic acid deficiencies were also clues to his underlying nutritional deficiencies.”
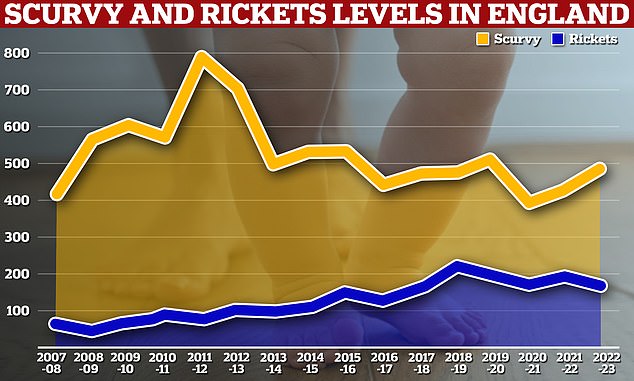
The statistics also showed that 171 people were treated for scurvy and 482 for rickets, with 405 of these patients being children.
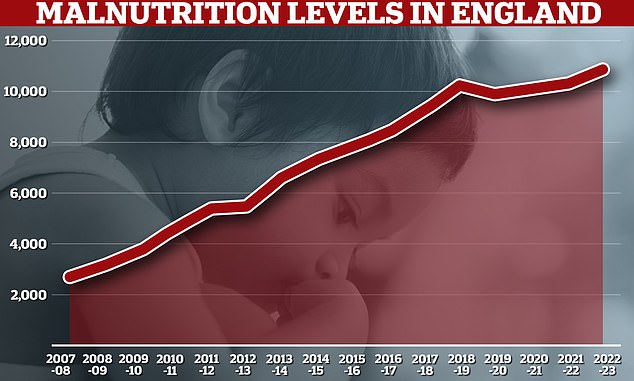
A Freedom of Information request from the Times Health Commission shows that 10,896 NHS patients in England were admitted to hospital with malnutrition in the year to April 2023. In 2007/2008 there were only about 2,700 hospital admissions due to malnutrition, rising to 5,500 in 2012/2013.
It is estimated that around 15 percent of adults in England use a proton pump inhibitor to treat conditions such as acid reflux and gastroesophageal reflux disease.
Scurvy and other conditions caused by malnutrition are also on the rise in Britain.
Doctors previously warned in the BMJ that there is a resurgence of scurvy because Britons are not eating enough fruit and vegetables.
In 2022, there were more than 800,000 admissions in England and Wales with conditions related to poor nutrition, including scurvy and rickets.
Nearly 11,000 people in England – including hundreds of children – were admitted to hospital with malnutrition in 2022.
Data from NHS England shows that the number of admissions due to the serious condition has quadrupled in the past 15 years and doubled in 10 years.
Medics have claimed that the cost of living is to blame for this.
Struggling Brits have been forced to cut back on fruit and vegetables and eat cheaper junk food, which lacks essential vitamins and minerals.
A Freedom of Information request from the Times Health Commission last year revealed that 10,896 NHS patients in England had been admitted to hospital with malnutrition in the year to April 2023.
Malnutrition occurs when a diet does not provide the right amount of nutrients, with unintentional weight loss, low body weight and feeling tired and weak being the main symptoms.
The statistics also showed that 171 people were treated for scurvy and 482 for rickets, with 405 of these patients being children.
Scurvy is caused by not consuming enough vitamin C, which is found in citrus fruits, broccoli and potatoes.
Typical symptoms include a feeling of fatigue, weakness and irritability, severe joint or leg pain and swollen and bleeding gums.
Adults ages 19 to 64 need 40 mg of vitamin C per day — about the amount in one orange — to help maintain healthy skin, bones and blood vessels.
