Doctors demand the NHS stops hiring lower-level medics and patients are told if they are not being seen by a fully trained medic
A revolt by senior medics will halt plans for the NHS to hire junior staff to plug NHS staff shortages.
Doctors said today that the healthcare industry is increasingly turning to physician assistants (PAs) because they are much faster and cheaper to train.
They warned that patients are often unaware that they are being seen by such staff, rather than a qualified doctor.
Associates do not go to medical school, but instead complete two years of postgraduate training on top of a degree in a subject such as biomedical sciences.
But the government wants to expand their role at the NS.
Doctors said today that the health care industry is increasingly turning to physician assistants because they can be trained much faster and cheaper. They warned that patients are often unaware that they are being seen by such staff, rather than a qualified doctor
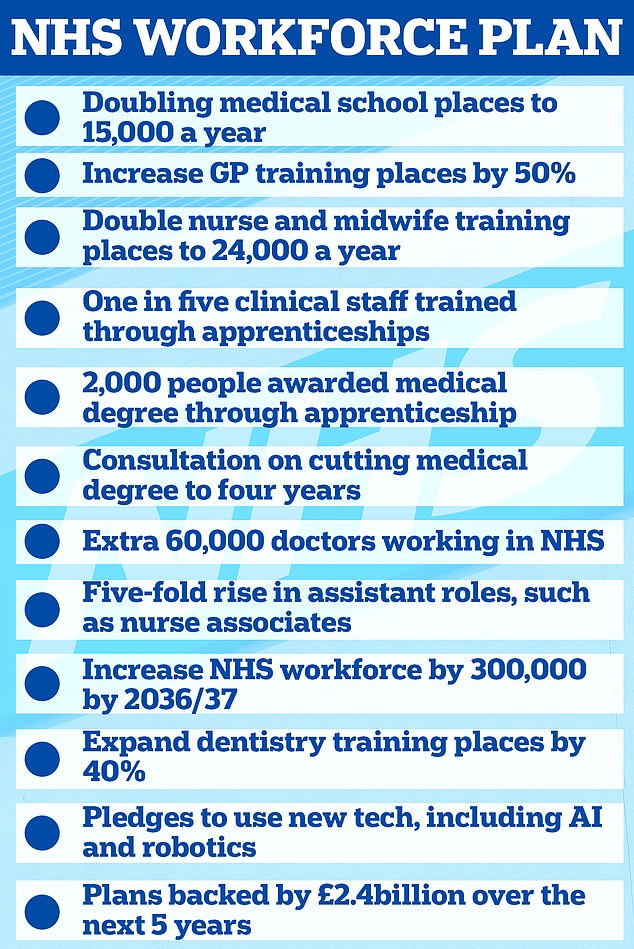
The plan, published in June, promises to increase the NHS’s permanent workforce by almost a million by 2036/2037. An increase is expected from 1.4 million to between 2.2 and 2.3 million. Under the NHS workforce plan published in June, ministers also plan to increase the number of PAs by almost four times to 12,000 by 2036/37. The plan also suggests that PAs may be allowed to prescribe medications in the future
Under the NHS workforce plan published in June, ministers plan to almost quadruple the number of them to 12,000 by 2036/2037.
The plan also suggests that PAs may be allowed to prescribe medications in the future.
This role was first introduced in 2003 and currently allows physician assistants to take medical histories, perform physical examinations and analyze test results, but they must always work under supervision.
They are not allowed to prescribe medications or refer patients for procedures.
The faculty, set up by the Royal College of Physicians, also says PAs are meant to work ‘alongside’ doctors and provide ‘medical care’.
However, in recent weeks concerns have increased about the scope of their role, public confusion about their level of expertise and the lack of regulation.
Senior anesthetists, under the group ‘Anaesthetics United’, have now also raised the alarm about their increasing use and called a general meeting of the Royal College of Anesthetists, in a bid to oppose plans for nurse anesthetists.
Employees may provide anesthesia under the supervision of a consultant, who may supervise two employees in separate operating rooms at the same time.
In theory, this allows more operations to be performed than if the consultant were to work directly on one patient.
Dr. Richard Marks, a semi-retired anesthetist in London, told the story The times: ‘Anaesthetists are non-physicians who have completed a two-year training course that enables them to provide anesthesia.
‘Theoretically under supervision and within limited practice, but anecdotally in the real world both conditions are waived.’
Consultant anesthetists normally undergo nine years of on-the-job training after medical school.
Dr. Marks, who has been both regional training director and vice-president of the Royal College of Anesthetists, also said arguments that associates were necessary given the national shortage of anesthetists ‘do not stand up to scrutiny’.
At a meeting scheduled for October 17, the group tabled motions, including a mandate for the university council to ask clinical directors to pause staff recruitment.
The group also insists that patients be told clearly when a staff member would provide their care.
The Times reported that similar efforts are in the early stages in other medical specialties, where physicians are deployed more frequently.
The government and the General Medical Council, which oversees doctors’ standards, have been discussing plans for staff to be regulated by the GMC for several years.
But the watchdog says this won’t happen until “the second half of 2024 at the earliest.”
The calls also come after the death of actress Emily Chesterton, who was just thirty.
In July it was revealed she had been seen twice by the same PA, who failed to notice the blood clotting symptoms and instead said the 30-year-old actress was suffering from anxiety and long Covid-19.
Her parents said that at no point during the GP surgery appointment was Mrs Chesterton informed that the person who diagnosed her was not a fully qualified GP.
Her health deteriorated on the same evening of her second appointment before her family called an ambulance, but last November she went into cardiac arrest on the way to hospital.

Under the NHS long-term workforce plan, the number of medical training places will be doubled by 2031/2032, bringing the total number of places to 15,000. GP training places in England for junior doctors will also increase by 50 per cent to 6,000. Training for pharmacists will also increase by almost 50 percent to around 5,000 places by 2031/32. Meanwhile, training for clinical psychology and child and youth psychotherapy will also be expanded, with the number of places increasing by more than a quarter to 1,300 in 2031

The calls also come after the death of actress Emily Chesterton (pictured), who was only 30. In July it was revealed she had been seen twice by the same PA, who failed to spot any blood clotting symptoms and instead said the 30-year-old actress had anxiety and long Covid. Her parents said that at no point during the GP surgery appointment was Mrs Chesterton informed that the person who diagnosed her was not a fully qualified GP.
A coroner concluded that her life could have been saved had she gone to the emergency room and been treated for a pulmonary embolism.
The GP practice where Ms Chesterton was seen, the Vale Practice in Crouch End, north London, now no longer employs PAs.
At the time, members of the doctors’ union, the British Medical Association (BMA), called for the role to be renamed ‘physician assistant’ and for greater efforts to ensure that medical assistants were not confused with doctors.
In the same month, at the BMA’s annual representative meeting in Liverpool, a motion was passed calling for the junior doctor to be renamed a junior doctor, and that those who fulfill this role in medical settings should never be referred to as ‘doctor’.
It also called on PAs to register through the Health Professions Council rather than the GMC, saying they must ‘take personal responsibility for their professional actions’.
Health Minister Will Quince said he would look into the suggestion for a new name and that whatever the title, “we need to make sure they represent themselves and their role appropriately, and make that very clear to patients.”
Dr. Fiona Donald, president of the Royal College, which surveys its members, said: ‘We are awaiting the results of our membership survey… There is enormous pressure on anesthesia services across the country due to a shortage of anesthetists and an unprecedented ask about our services. and a lack of training places for doctors specialized in anesthesia.’
Meanwhile, an NHS spokeswoman said: ‘Anesthetist nurses are highly trained practitioners who work under the supervision of a consultant… helping to free up doctors so they can spend more time with patients.’
