Diabetes-related amputations and complications cost the NHS £6 billion annually
The NHS spends £6 billion a year on diabetes-related complications such as amputations and blindness, an alarming report has found.
Diabetes UK warns that many of the problems are avoidable and calls on the health service to shift its focus ‘from crisis to preventive care’.
The charity says this would reduce harm to patients living with the condition and reduce the extraordinarily high costs.
Diabetes UK estimates that more than 4.4 million people in Britain are living with diabetes, and a further 1.2 million may have undiagnosed type 2 diabetes, which is linked to obesity.
Every week, diabetes leads to 2,990 cases of heart failure, more than 930 strokes, 660 heart attacks and 184 amputations.
Kim Steer, 56, from Yeovil, Somerset, was diagnosed with type 1 diabetes when she was 19. She has diabetic retinopathy, an eye disease that occurs when your blood sugar and blood pressure are consistently high
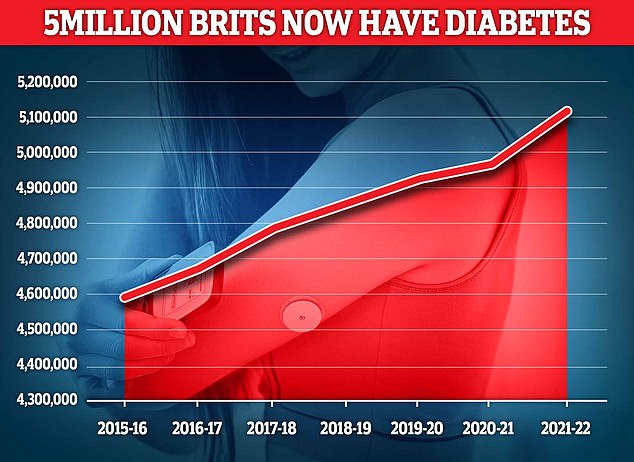
Nearly 4.3 million people were living with diabetes in 2021/22, according to the latest figures for Britain. And another 850,000 people have diabetes and are completely unaware of it, which is worrying because untreated type 2 diabetes can lead to complications including heart disease and stroke.
To reduce the risk of complications, patients should self-manage their condition, with regular support from healthcare professionals.
However, figures show that 1.6 million people with diabetes in England will not have received all eight checks they were entitled to in 2022/2023.
New research commissioned by Diabetes UK – and conducted by economists at the University of York – estimates that the direct cost of diabetes to the NHS in 2021/2022 was £10.7 billion.
This was equivalent to 6 percent of the total UK healthcare budget and more than £9.8 billion in 2012.
About 80 percent of these costs were due to diabetes-related complications, such as problems with the kidneys, eyes, circulation and nerve damage in 2012.
Improvements in blood sugar control have reduced this figure to 60 per cent in 2021, the latest year available, but it still means the NHS is spending £6.2 billion a year on ‘potentially preventable complications’, according to Diabetes UK.
The rest, around £4.4 billion, was spent on diagnosis, GP appointments, eye tests, blood tests, medication, support programs and a specialist diabetes team.
Academics urged health officials to ‘continue investing in the prevention, care and treatment of diabetes to reduce the future costs of complications with population-level interventions, in addition to individual approaches’.
And they warned that the total annual cost to the NHS could rise to £18 billion by 2035 if action is not taken to reduce the number of people developing type 2 diabetes and improve outcomes for everyone living with the disease.
Colette Marshall, CEO of Diabetes UK, said the research ‘paints a grim picture’.
“These complications cause untold hardship for many thousands of people and are in most cases preventable with proper care,” she added. “Getting the right care for people with diabetes can save limbs, vision and lives.
‘But despite some progress, too many people still miss the disease and too many develop diabetes complications.
‘Switching the dial from crisis to preventive care would help reduce the harms of diabetes, allowing people with the condition to live well and ultimately reducing healthcare costs.’
Last year, academics said diabetes cases were likely to ‘grow aggressively’ in every country and among every age group.
An article published in the journal Lancet Diabetes and Endocrinology states that approximately 1.3 billion people will have diabetes by 2050, more than double the 529 million cases in 2021.
Earlier this month, NHS England chief executive Amanda Pritchard said the number of people under 40 at risk of developing type 2 diabetes rose by a quarter last year.
The latest National Diabetes Audit found that by 2023, 3.6 million patients registered with a GP had pre-diabetes – when blood sugar levels are above the normal range, but not high enough to be diagnosed.
This is an increase of 549,000, or 18 percent, compared to the previous twelve months.
Among young people under 40, this figure rose by almost a quarter, from 173,166 in 2022 to 216,440 last year.
Nick Hex, associate director for the NHS and public sector at the York Health Economics Consortium, said: ‘Diabetes is a debilitating and serious condition that affects people on many different levels every day.
‘It remains very expensive for the NHS, and the majority of that cost continues to be spent on potentially avoidable complications.
‘Increased investment in new medicines and technologies that help people better manage their condition is contributing to some of the high ongoing costs, but the rise in type 2 diabetes under 40s is of particular concern and there needs to be continued attention to prevention strategies.’
