Colorado veterans hospital STOPPED heart surgeries for a year due to ‘exodus’ of surgeons pushed out by ‘culture of fear’
A veterans hospital has been accused of endangering heart patients after life-saving heart surgeries were halted for a year due to a catastrophic staffing shortage, multiple investigations have found.
Two government investigations found a “culture of fear” at the Rocky Mountain Regional VA Medical Center in Colorado, where leaders “humiliated” and “swore” at staff, causing more than two dozen top doctors, nurses and support staff to resign between 2020 and 2023.
The hospital, which treated more than 100,000 veterans a year, is accused of violating protocol by failing to disclose to officials the years-long halt to the procedures.
One of the studies involved the case of a 72-year-old man who died of cardiac arrest because no suitable heart specialist was available to monitor him.
The reports show the regional VA medical center served 101,400 patients between October 2022 and September 2023
The investigation, conducted by the U.S. Department of Veterans Affairs Office of the Inspector General (OIG), included interviews with more than 50 former and current employees.
There are 172 VA medical centers and 1,138 VA outpatient clinics across the country, providing care to approximately 6.8 million veterans annually.
From October 2022 to September 2023, 101,400 of these veterans received care at the Aurora-based Rocky Mountain facility – the same period OIG investigators focused on.
Concerns about the state of the nation’s VA health care system have existed since the 1990s, he said a review from 2023 from the David Geffen School of Medicine at UCLA and the VHA.
They included criticisms that the quality of care was inconsistent and unpredictable and that services were expensive and difficult to access.
In 2014, Congress passed a law addressing some of these concerns. This allows veterans who had to wait longer than 30 days for care or who lived 40 miles from the nearest VA center to go to local hospitals and get their care reimbursed.
This was followed by a 2018 law that created a long-term benefits program for veterans who had VA insurance and did not have easy access to VA hospitals or clinics.
In the case of the Colorado hospital, the reports noted that staffing shortages contributed to the years-long gap in cardiac care.
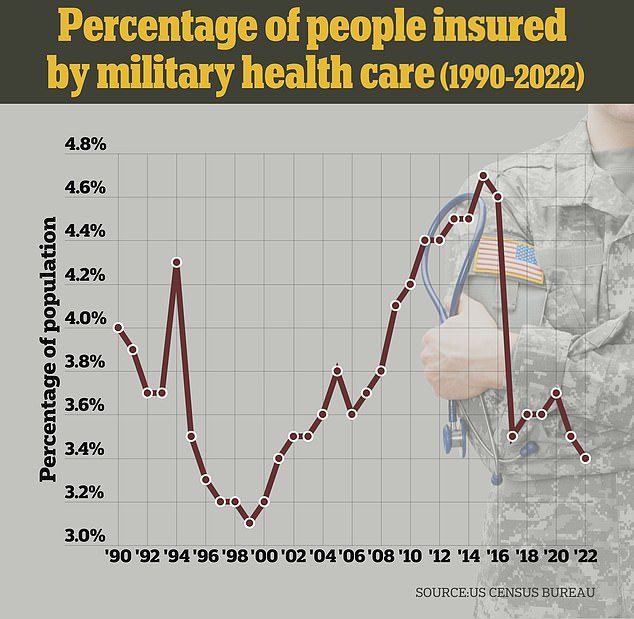
In 2022, about 3.5 percent of all Americans received their health care through military programs, down from 4.7 percent in 2015.
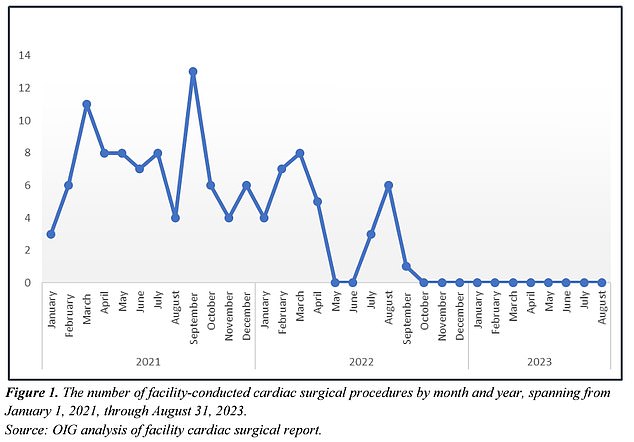
The initial investigation found that hospital officials first stopped performing heart surgeries in June 2022 after five ICU nurses, who were critical to monitoring patients undergoing heart surgery, quit.
Management informed the authorities of this interruption and resumed work a month later.
But in September 2022 they stopped again. That pause lasted until October 2023. During this time, three of the hospital’s four cardiac surgeons quit and the last was fired.
During this period, patients continued to come in needing care, but the lack of organization and staff created confusion.
Seven healthcare providers reported on the 72-year-old man’s story, saying his death was an example of the hospital’s “unclear guidelines.”
The man was admitted to the Rocky Mountain Intensive Care Unit early 2023 with shortness of breath and an irregular heartbeat. It was soon discovered he was showing signs of heart failure.
The report states that two different doctors recommended two different courses of treatment.
The patient rapidly deteriorated and went into cardiac arrest, but the ICU staff had no cardiac specialists in the hospital to address his poor health – and resorted to consulting a cardiologist via telehealth.
OIG officials wrote that the patient died despite the efforts of intensive care unit staff, who were left to care for the man only on the advice of a telehealth cardiologist.
The report stated that This situation illustrates how ‘unclear government guidelines’ have ‘put patients at risk of adverse clinical outcomes.’
An anonymous ICU physician told researchers that the advice from the virtual consultation specialist was “not helpful.”
More layoffs followed later that year, with the deputy chiefs of anesthesiology, general surgery and mental health all leaving the eastern Colorado hospital.
The second study captured the majority of cultural issues within the Colorado hospital in four roles: the facility director, the chief of staff, the deputy chief of staff for inpatient operations, and the deputy chief of staff for education.
In an anonymous interview, a doctor told investigators that during a last-minute town hall meeting in 2023, the facility’s chief of staff and director “just scolded us for going outside the hierarchy…
“…what was ostensibly a town hall meeting was them targeting us for reaching beyond our chain of command.”
Investigators concluded that the executive staffers had created “widespread disenfranchisement and a culture of fear,” leading to the firings.
A separate, anonymous psychologist working at the hospital described “There was stress among staff, leading to an ‘exodus’ of qualified personnel at all levels, which in turn harmed veteran care.”
Because staff felt they could not speak out without fear of reprisal, they were reluctant to carry out risky but necessary procedures, the report said, adding that leadership had used reports of safety problems as “a way to assign blame.”

The 1.2 million square foot hospital was completed in 2019. Construction, which cost the Army Corps of Engineers $1.7 billion, began in 2014
The OIG report states that new leadership staff plans to address these concerns by hosting “listening sessions” to promote a healthier hospital culture. The Denver Post reported.
Sunina Kumarthe CEO of the VA Rocky Mountain Network, which oversees veterans hospitals in Colorado, Oklahoma and Utah, thanked the OIG for its investigation in a public statement.
When asked for comment on this story, VA representatives told DailyMail.com that Ms. Kumar said: ‘These investigations will ensure that veterans, employees and stakeholders have full confidence in the quality and integrity of leadership and the care provided. ‘
There have been major leadership changes at the organization over the past year, and the report says interim leaders are addressing these issues.
On a larger scale, the OIG report recommended that the federal VHA increase oversight of its hospitals — including conducting leadership assessments, conducting exit interviews with employees and establishing a feedback system that allows employees to share their concerns.
Local VA leaders, like Ms. Kumar, appear to be accepting the change.
“The VA OIG has released two reports that show we have work to do here and I am fully committed to rebuilding trust with the veterans we serve,” Ms. Kumar said.

Sunaina Kumar, the Chief Executive Officer of the VA Rocky Mountain Network, thanked the OIG for its investigation
Even with increased attention to the national VA health care system in recent decades, there are still national disparities between veterans who use VA care and those who choose private providers.
Under this system, veterans can apply for health care benefits through the Department of Veterans Affairs’ Civilian Health and Medical Program.
It covers health care services and supplies for veterans at all VA medical centers, but generally does not cover services offered at outside medical clinics.
Veterans can also still choose to use private insurers for their care.
Veterans who use VA services tend to be less healthy than veterans who use private health care. According to a 2015 report by the RAND Corporationa think tank that advises on US government policy.
Veterans across the country are also struggling to get the care they need from VA hospitals. A 2021 study of 8,670 military families reported that their top concern was access to care from the VA.
Approximately 9.2 million veterans use this health care system, about half of all living veterans.
Respondents said difficulty scheduling appointments, accessing the right care and poor quality of care were the top barriers to getting the help they needed.
In a separate one Survey Mission Roll Call 2021 It was determined that there were not enough appointments available, whether for heart surgery or mental health care, for the 16.5 million veterans living in America in 2021.
