CDC issues urgent warning about six ‘silent killers’ emerging in US, including incurable deadly fungal disease
Health authorities are raising alarms over the emergence of six “silent killers” in the US that are becoming resistant to the drugs normally used to treat them.
A new CDC report A study on the threats from antimicrobial resistance found that infections with six difficult-to-treat germs increased by at least 20 percent during the Covid pandemic compared with 2019. Infections remained high through 2022, the most recent annual data available.
Of particular concern was the emergence of an antifungal-resistant fungus that can cause serious illness and often spreads in healthcare settings, Candida auris, which increased fivefold from 2019 to 2022.
Officials estimate that 29,400 people died from antibiotic-resistant infections in 2020, but admit that is likely a large underestimate due to underreporting. They also say the 2019 count of 35,000 deaths per year was likely more accurate.
This increase raises concerns that deaths from these once treatable germs will increase because the drugs used to treat them no longer work.
Lorrie McCreary, 86, contracted Candida auris when she was transferred to a rehabilitation unit at Baycare St Anthony’s Hospital in St. Petersburg, Florida
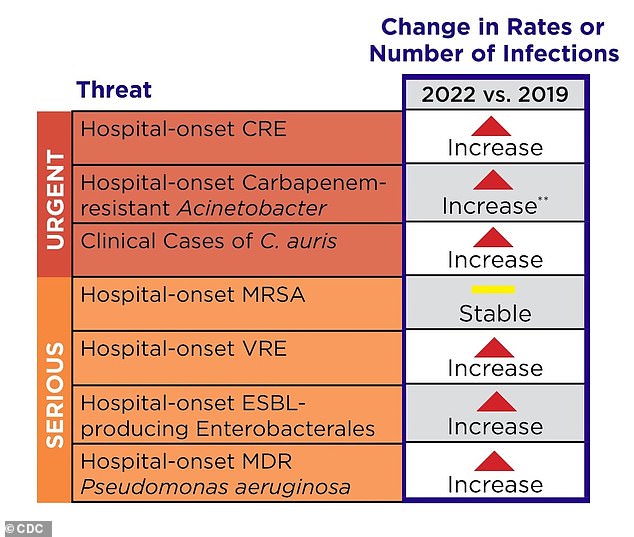
The table above shows how the number of infections in the US has shifted between 2019 and 2022
Infections that are resistant to antibiotics cannot be treated with standard medications.
The CDC’s latest report looked at seven hospital pathogens and found that infections in six of them were elevated compared to years before the Covid pandemic.
Of the six, five are resistant bacteria and one is a resistant fungus.
These include Carbapenem-resistant Enterobacterales (CRE), carbapenem-resistant Acinetobacter, Vancomycin-resistant Enterococcus (VRE), Extended-spectrum beta-lactamase (ESBL), multi-resistant Pseudomonas aeruginosa and Candida auris (C. auris).
MRSA was the only resistant pathogen of the seven whose number of cases remained stable between 2019 and 2022.
Poor infection control measures, such as not washing hands or not changing personal protective equipment between patients, lead to the risk of these bacteria spreading within a hospital and even beyond.
In addition, overuse of antibiotics increases the chance that pathogens will become resistant. This is because resistant strains survive longer and can spread more easily, because other, non-resistant types are eliminated.
The CDC wrote in its report: “The pandemic has reversed much of the progress the country has made against antimicrobial resistance, particularly in hospitals.
“The US must continue to invest in preventive public health measures to combat antimicrobial resistance.”
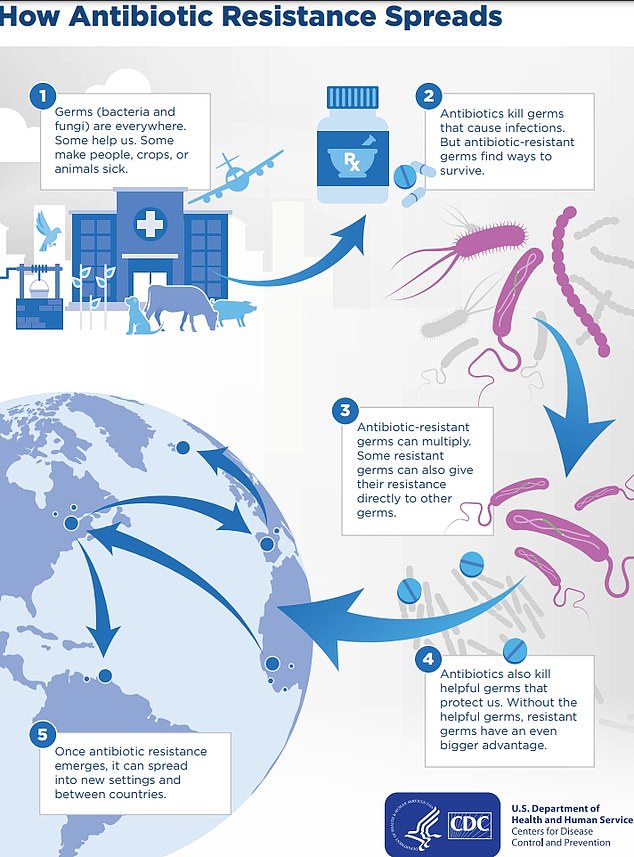
The above shows how antibiotic resistant infections are spreading in the US and between countries
Officials said COVID-19 may have caused the increase due to longer hospital stays, shortages and increased pressure on staff and resources, and disrupted infection control measures.
They said these measures would make it easier for multi-resistant bacteria to spread in hospitals, increasing the risk of more infections.
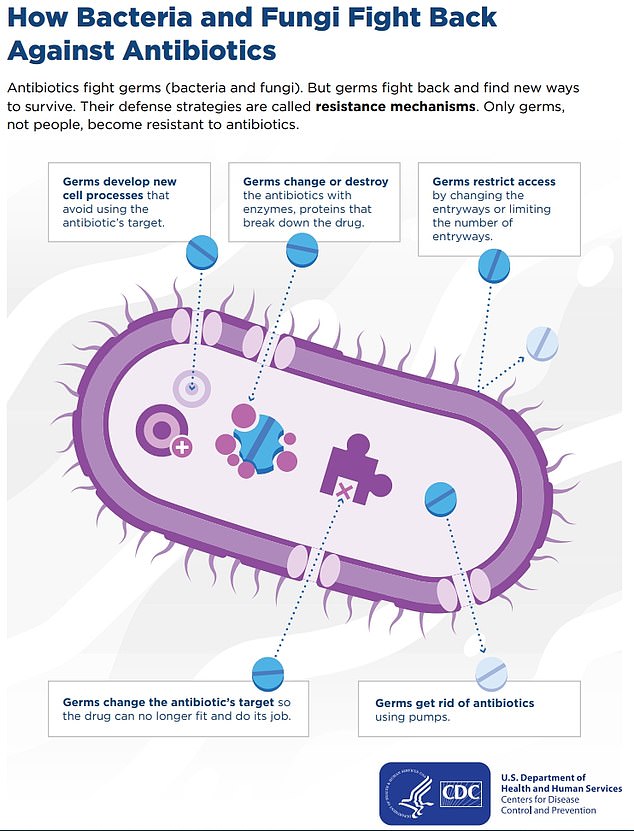
The above shows how a bacterium or fungus can fight an antibiotic and acquire immunity, making the drug redundant.
Officials were particularly concerned about the fungus C. auris, which can cause sepsis, saying the number of cases nearly increased fivefold during the same period.
Sepsis is a life-threatening condition that occurs when the body’s immune system overreacts to an infection, causing severe inflammation that causes organ failure.
About a third of patients with this condition do not survive.
One of the patients who contracted C. auris as a result of the pandemic was Lorrie McCreary, who died from the infection in June 2022.
The 86-year-old was admitted to hospital with pneumonia and appeared to be recovering well.
However, her condition deteriorated rapidly, prompting her doctor to run a series of tests which revealed she had a fungus, which she is believed to have contracted in hospital, probably through an oxygen tube.
It caused a series of fatal events, leading to sepsis, kidney failure and a fatal stroke.
Her daughter Sharon, 61, said she felt her mother would still be alive if she had not contracted the infection.
Data shows that there are more than 80,000 cases of MRSA and 11,000 deaths in the US each year.
For the report, the CDC analyzed data on seven antibiotic-resistant infections provided by hospitals and labs across the country.
The report also found that during the Covid pandemic, nearly 80 percent of hospitalized Covid patients from March to October 2020 received an antibiotic.
Officials said this was initially due to the difficulty in distinguishing between Covid and community-acquired pneumonia in the early days.
But antibiotics don’t work against Covid because they are specifically designed to target bacteria and not a virus.
