Breast cancer patients could soon get a BIONIC BREAST that brings back sensation in the chest after a mastectomy
>
Scientists are developing an “electronic breast” device that can restore the sense of touch in breast cancer survivors undergoing mastectomies and reconstructive surgeries.
The implantable device developed by researchers at the University of Chicago could benefit the approximately 3.5 million breast cancer survivors in the United States who have undergone a mastectomy to prevent breast cancer from recurring or spreading to other parts of the body.
Many people who undergo this surgery, in which one or both breasts are removed and often followed by breast implants, lose sensation in their chests, which experts say can cause a significant loss of sense of self and hinder a woman’s sexual satisfaction.
Flexible sensors will be inserted into the women’s chest in two stages, during the initial mastectomy and then during reconstructive surgery using implants or tissue from the woman’s own body, which will be connected to electrodes placed in the armpits.
When the breast is placed under any kind of pressure, which could be from someone’s hug or during intimacy, the electrodes send signals to the nerves running between the ribs, which the brain interprets as sensation.
The chart above shows new breast cancer cases among women as a rate per 100,000 people (light green line) and death rates (dark green line). It reveals that deaths are decreasing very gradually
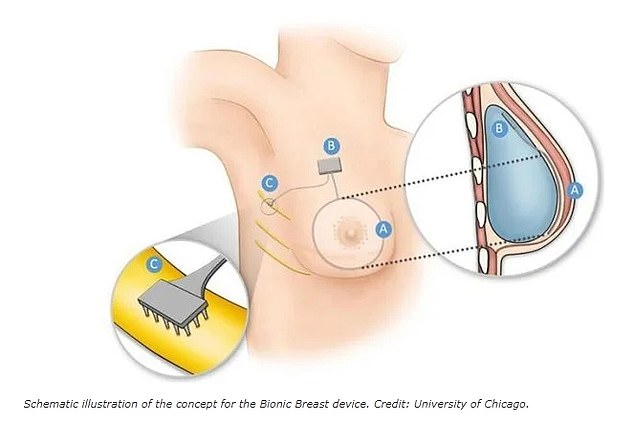
The photo shows how the “electronic breast” will work. The pressure sensors (A) will be connected to a circuit inside the breast implant (B) which connects to the implanted electrodes (C) under the arm. The electrodes are then connected to the intercostal nerves that supply the breast
Breast cancer is the second leading cause of cancer death among women, claiming the lives of 42,000 women every year.
Mastectomies are effective in preventing cancer from returning, but women who undergo these procedures often experience the same sense of physical and existential loss as amputees.
This advanced technology is based on the work carried out by University of Chicago researcher Dr. Suleiman Ben Samia, who passed away in August.
Dr. Ben Smaia has been working on a way to develop prosthetics that can restore a realistic sense of touch to amputees and paralyzed patients.
Dr. Stacy Tesler Lindau, a professor of obstetrics and gynecology at the University of Chicago, is collaborating with neuroscientists and biomedical engineers to advance Dr. Bensamaya’s work in leveraging technology to restore neural sensation to the reconstructed breast.
“Even if their breasts are cosmetically reconstructed, women still have many of the same experiences as someone who loses a limb, such as feeling like they are no longer part of their body, complete loss of sensation and even pain,” Dr. Lindau said.
For many people, it is not just a physical loss, but a psychological and even existential loss as well.
The first-of-its-kind implantable device aims to restore a woman’s mental health and sense of self that she can lose after undergoing breast removal surgery and while recovering from cancer.
The implantable sensor will be inserted under the nipple of the reconstructed breast and connected to electrodes implanted near the armpit. The electrodes are then connected to the branches of the intercostal nerves located under the ribs.
The ultimate goal is to restore response to touch, movement, pressure, and other stimuli by triggering signals to the brain that interprets those signals as sensations.
The implantable sensor would be flexible and soft, like human tissue, so that it would respond to even simple movements that squeeze or flex the breasts, such as taking a deep breath, hugging a loved one, or engaging in sexual intercourse with a partner.
It will also be important for the team and the device’s lead developer, Dr. Sihong Wang, to ensure that the patient’s immune system will not reject the transplant, which can happen after organ transplants.
“Natural movements that bring about changes in the shape of the muscles and skin will also bring about changes in the sensor,” Dr. Wang said.
“The overall goal is to create a sensor that is soft and flexible like biological tissue, but with a chemical design that is compatible with the immune system that we can leave in the patient’s body for the rest of their life.”

The implanted device could benefit the approximately 3.5 million breast cancer survivors in the United States who undergo mastectomy to prevent cancer from spreading to other parts of the body or coming back after bouts of remission.
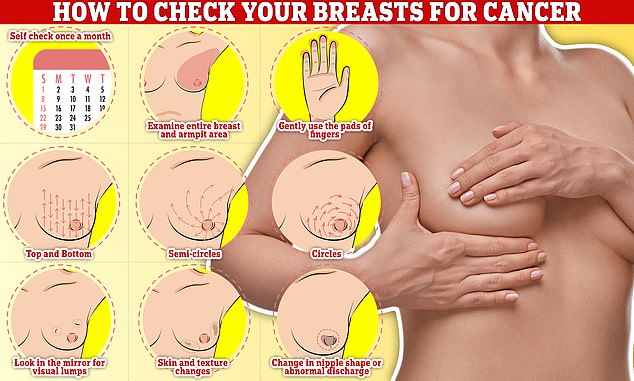
Examining your breasts should be part of your monthly routine so you notice any unusual changes. Simply rub and feel from top to bottom, feeling in a semicircle and in a circular motion around the breast tissue to feel for any abnormalities.
The team received a $4 million grant from the National Institutes of Health to make the device and launch a human trial in patients about to undergo a mastectomy.
The plan is to implant the device in two stages, during the mastectomy and then during the first stage of reconstructive surgery.
The National Institutes of Health will largely move toward creating the device and conducting proof-of-concept testing.
Before the second phase of reconstructive surgeries, patients will visit a laboratory where researchers will test the device by delivering electrical pulses via electrodes.
Patients will report the sensations they feel and any pain or discomfort so researchers can fine-tune the devices accordingly. Then, in the second stage of reconstructive surgery, the hardware will be removed.
If these devices prove proof of concept, they are expected to be trialled on a larger population of humans, at which point they may remain implanted in the breasts for a longer period.
Dr. Lindau said she came up with the idea for the “bionic breast” after meeting with patients who discussed loss of sexual function after mastectomies and reconstructive surgery.
Her team is currently interviewing women about their concerns after surgery and interactions with their doctors about what to expect.
“We interview people who say, ‘I want the surgeon to clearly tell me that most of the nerves are surgically removed along with the breast,'” Dr. Lindau said.
“One patient reported that her surgeon talked to her for 20 minutes before he mentioned the word nipple. Patients want open but compassionate communication while recognizing that what is lost is not just sensation in the breast, but also the functioning of an important sexual organ.”
Thanks to advances in preventive measures such as mammograms, breast cancer death rates have fallen by more than 40 percent since the 1990s.
But cases rise each year by about 0.5 percent. In 2023, an estimated 298,000 women will be diagnosed with invasive breast cancer for the first time, and more than 43,000 women will die.
(tags for translation) Daily Mail
