Alzheimer’s may be able to SPREAD to organ transplant patients, study suggests – as experts call for dementia screening for ALL donors
- Researchers in Canada suggested that Alzheimer’s disease could be spreading in mice
- The spread came from bone marrow transplants containing defective genes
- READ MORE: NIH Launches Urgent Study on Whether Alzheimer’s Disease Can Spread
Alzheimer’s disease could spread to patients who receive transplants containing potentially toxic genes, a study suggests.
Researchers in Canada are now calling for all donors to be screened for the disease, in case cases go undetected.
The new study looked at mice that had stem cells transplanted from their bone marrow from donors with familial Alzheimer’s disease.
This type is caused by a single genetic mutation passed down through families and affects almost 350,000 Americans and 1 percent of Alzheimer’s cases in Britain.
Researchers in Canada found that mice that received bone marrow transplants containing stem cells with defective genes developed Alzheimer’s disease more quickly than mice that did not.
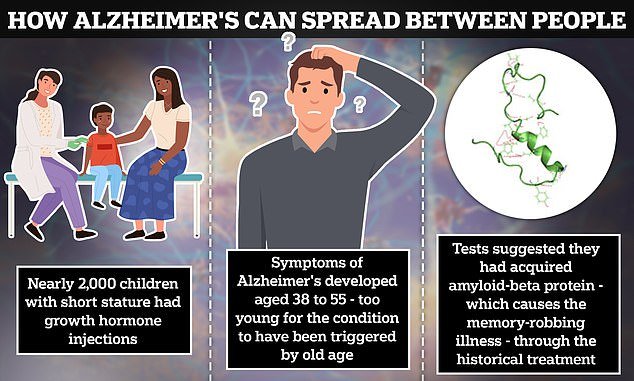
A British study evaluated five patients injected with growth hormones as children who were infected with toxic amyloid beta protein ‘seeds’. All five suffered from the same rare early form of the devastating dementia. Others who received the same treatment are now considered ‘high risk’
Patients with this form of Alzheimer’s disease carry a defective version of the amyloid precursor protein (APP) gene, which can turn into plaques and affect the brain.
For the first time, the study appeared to show that this process starts outside the central nervous system and then moves to the brain, where it causes the cognitive decline associated with Alzheimer’s disease.
The team found that the mice showed signs of cognitive decline as early as six months of age – in almost half the cases of those that had not undergone a transplant.
The study comes amid overwhelming evidence from Britain showing that at least five people “contracted” the memory-robbing disorder from a now-banned hormone treatment that was contaminated with toxic proteins from the bodies of sick people.
The authors of the new study called for blood, tissue and organ donors to be screened for Alzheimer’s disease to prevent possible spread of the disease.
But they noted that more research is needed to see if the effect is the same in humans and other species.
Dr. Wilfred Jefferies, senior study author and immunologist at the University of British Columbia, said: ‘This supports the idea that Alzheimer’s disease is a systemic disease in which amyloids expressed outside the brain contribute to the pathology of the central nervous system.’
‘While we continue to investigate this mechanism, Alzheimer’s disease may be the tip of the iceberg and we need much better monitoring and screening of the donors used in blood, organ and tissue transplants, as well as in the transfer of from humans derived stem cells. or blood products.’
It is unclear whether any cases of Alzheimer’s have yet been linked to organ or bone marrow donations.
The new study was published in the journal on Thursday Stem cell reports.
Researchers transplanted bone marrow – a spongy substance in the center of the bones – with stem cells containing APP into two different groups of mice: mice without the APP gene (APP Knockouts) and mice with a normally functioning gene.
They found that mice with a normally functioning APP gene developed signs of cognitive decline in nine months, and mice without the gene showed features of Alzheimer’s disease in just six months.
Normally, mice susceptible to familial Alzheimer’s begin showing symptoms around 11 to 12 months of age.
In mice, these symptoms usually include loss of short- and long-term memory and an absence of anxiety. Signs in the brain include a buildup of amyloid in the brain and leaks in the blood-brain barrier.
Dr. Chaahat Singh, lead author of the study and a neuroscientist at the University of British Columbia, said: ‘The fact that we were able to see significant behavioral differences and cognitive decline in the APP knockouts after six months was surprising but also intriguing because it only appearance of the disease that accelerated after transmission.’
The findings suggest that the mutated APP gene in donor stem cells could cause the disease in people without the gene and that people with a normal APP gene are more susceptible to it.
The team also concluded that Alzheimer’s disease may arise from amyloid proteins found outside the central nervous system.
The findings come after a British study found evidence that at least five patients who were injected with growth hormones containing ‘seeds’ of amyloid beta protein – harvested from the bodies of dead people – ‘contracted’ Alzheimer’s disease later in life .
More than 1,800 other patients who received the treatment were considered ‘high risk’.
An NIH panel announced in January that it would launch an “urgent” investigation into the research, as nearly 8,000 American children were injected with the therapy between the 1960s and 1980s.
