AI is better than doctors at detecting prostate cancer on MRI and can reduce unnecessary surgeries
Artificial intelligence is better at detecting prostate cancer than hospital doctors, according to a groundbreaking study.
The computer system was developed by experts and has been trained and then tested on more than 10,000 prostate MRI examinations in patients.
Using the AI resulted in half the number of false positives and reduced the number of clinically insignificant cancers by a fifth compared to radiologists, the study found.
Doctors believe this could help reduce overdiagnosis and prevent unnecessary surgery for the most common cancer in men, which could be a major benefit to any future screening program.
Researchers predict that using AI to help read scans will be crucial in tackling the rising demand for medical imaging worldwide.
The computer system was trained and then tested on more than 10,000 MRI examinations of the prostate in patients
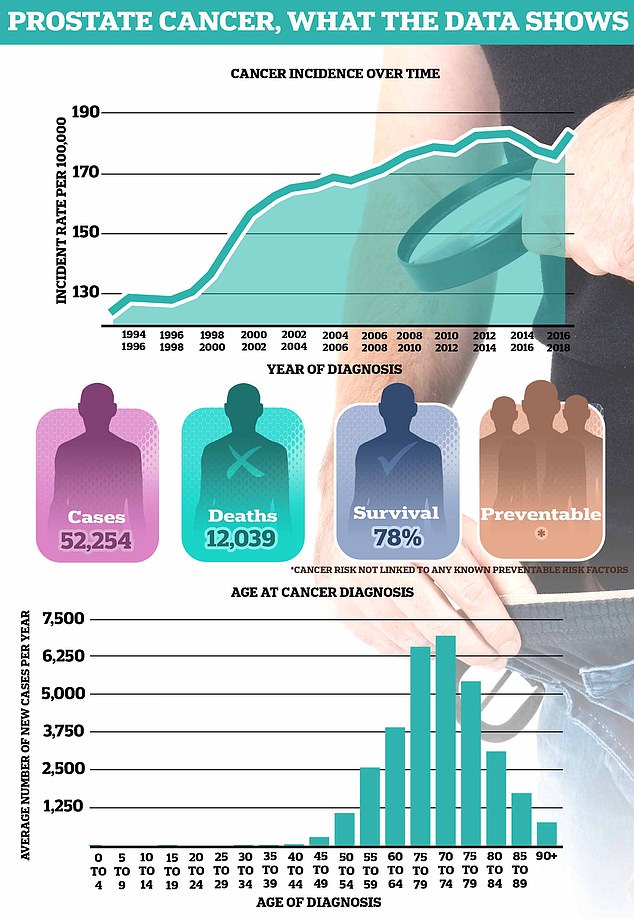
On average, more than 52,000 men are diagnosed with prostate cancer every year in the UK, making it the most common form of cancer in men. About 12,000 men die from the disease every year – the equivalent of one man every 45 minutes
However, there is limited scientific evidence so far on whether it really works, which is holding back the widespread adoption of AI systems for prostate cancer diagnosis.
They wanted to test whether state-of-the-art AI models, trained using thousands of patient surveys, were as good as radiologists at detecting clinically significant prostate cancer using MRI.
In the first study of its kind, an international team developed the technology using 10,207 MRI examinations of 9,129 patients in the Netherlands.
This was then tested on a further 1,000 scans of patients to determine whether the men had cancer and if so, how aggressive it was likely to be.
The technology competed against 62 radiologists from 20 countries, each with an average of five to 10 years of experience interpreting prostate MRI scans.
The diagnoses were then tested against the results using histopathology – analysis of cells under the microscope – and how the patients fared on average four to six years later.
It was found to be as effective as radiologists at detecting more serious prostate cancers and gave half the number of false positives, which can lead to unnecessary biopsies.
AI also picked up 20 percent fewer cases where the cancer was so low that it was unlikely to affect the patient during their lifetime, according to the paper published in The Lancet Oncology.
The global researchers, including from Radboud University Medical Center, Netherlands, conclude: ‘AI systems, when adequately trained and validated on a target population with thousands of patient cases, can potentially support the diagnostic pathway of prostate cancer treatment.
“A clinical trial is needed to determine whether such a system translates into improvements in workflow efficiency, healthcare equity and patient outcomes.”
It comes as a ground-breaking trial into prostate cancer screening is launched in Britain, and a national screening program is likely to follow.
Transform will test the effectiveness of diagnostic techniques, including MRIs, compared to the current standard blood test for prostate-specific antigen (PSA).
Prostate cancer is the most common cancer in men and the second deadliest, responsible for approximately 12,000 deaths per year.
The earlier the diagnosis is made, the better the results; the majority of men are still alive five years later if diagnosed at the earliest stages, compared to only half at stage four, when the disease has spread elsewhere.
Late diagnosis is also extremely expensive for the NHS, with hormone treatments for advanced prostate cancer estimated to cost tens of millions per year.
Last year, the European Council agreed on a recommendation that countries should consider the feasibility and effectiveness of prostate cancer screening based on PSA testing followed by an MRI scan.
Prostate Cancer UK is now calling on GPs to actively target high-risk men – such as those with a history of cancer in the family or black men – to see if they want a PSA blood test.
The charity wants other trained healthcare professionals, such as practice nurses, to be trained in advising men about the disease and testing options.
Chiara De Biase, Director of Health Services, Equity & Improvement at Prostate Cancer UK, said: ‘We know that many men don’t come forward because they think they will be invited as part of routine testing – when this is simply not the case. it’s true.
‘The long-term answer is a screening program for all men, and the results of our TRANSFORM study will tell us the most effective way to do that.
‘Until then, we must all work together to ensure men know what their risk is and what they can do about it.’

