My son had ‘unnecessary’ surgery at age 2 – it went wrong and he has been on life support for six years
A little boy has been in a vegetative state for six years after his brain was deprived of oxygen during an operation his family said was unnecessary.
Carlos Blanco, now eight, was born with subglottic stenosis, a narrow airway that can cause babies to produce a whistling sound while breathing or become short of breath.
While many children are advised to wait and grow out of this, the Blanco family was told their son needed surgery to widen his windpipe.
But during the operation, Carlos, who was two at the time, suffered cardiac arrest, cutting off blood flow to his brain.
After doctors finally managed to restart his heart, he had suffered severe brain damage as the lack of oxygen had caused brain cells to die.
His family is now suing his doctors and the New Mexico hospital, claiming their actions robbed the boy of his young life and caused “significant, debilitating and permanent injuries.”
Carlos Blanco pictured before undergoing surgery at the age of two
Carlos barely survives today and can only breathe through a machine that requires constant monitoring and cleaning.
He has his eyes open, but cannot talk, walk, eat alone, dress, go to the toilet or do anything that a young boy his age would normally do.
Carlos’ case was revealed in court records in the 1st Judicial District in Santa Fe, New Mexico.
The toddler had undergone two procedures to widen his airway at Presbyterian Hospital in Albuquerque, New Mexico, in April and June 2018, both of which were successful.
But after he developed a new cough, his surgeon Dr. Jonathan Owens, who lived in Las Cruces, New Mexico – close to the family’s home, that he would undergo a third surgery in September of that same year.
Dr. Owens offered to perform the surgery himself so the family wouldn’t have to travel to Albuquerque, some 200 miles away, for a third time – which they agreed to.
According to court records, the then two-year-old suffered cardiac arrest – or a medical emergency in which the heart stopped beating – during this procedure.
Doctors performed CPR, but Carlos’ brain was deprived of oxygen for too long, causing serious damage. He was diagnosed with an anoxic brain injury.
Court records show the cardiac arrest was “mismanaged” for 15 minutes, during which CPR was performed and medications were administered.
Brain tissue is very sensitive to an interruption of oxygen supply and brain cells begin to die within minutes of low oxygen levels, according to the Cleveland Clinic.
After his heart restarted, doctors discovered that Carlos could not breathe on his own and the toddler had to be placed on a ventilator for 13 days.
After two weeks, doctors performed a tracheostomy, a procedure that creates an opening in the throat through which a tube can be inserted so a person can breathe.
Carlos was discharged from his mother Josefina Blanco on October 9, 2018, and later returned home, where he has been in a vegetative state ever since.

After the surgery, Carlos – pictured above before the surgery – was left in a vegetative state
Carlos is not expected to recover and he now requires 24-hour care and a machine to breathe.
Carlos’ mother is suing the hospital, Memorial Medical Center in Las Cruces, New Mexico, and Dr. Owens, an otolaryngologist (also known as an otolaryngologist) who recommended and performed the surgery, for medical malpractice.
She is seeking an undisclosed amount for her son’s “significant, disabling and permanent injuries.”
Attorney Adrian Vega, who represents Carlos and Josefina, said in a statement: “In this case, we have a little boy in a vegetative state who requires 24/7 care.
“(Subglottic stenosis) is an airway problem that generally resolves in most children once they reach toddler status, so they actually grow older.”
In a statement to the Las Cruces Sun Newsa Memorial Medical Center spokesperson said, “As a matter of practice, MMC does not comment on active litigation and federal law prohibits us from discussing specific patient issues.”
Memorial Medical Center and Dr. Owens did not respond to DailyMail.com’s requests for comment.
Carlos, a twin, had mild to moderate subglottic stenosis, which caused him breathing problems but did not result in frequent hospital admissions, a source close to the case told DailyMail.com.
There are no formal guidelines on whether children with a mild form of the condition should undergo surgery, but doctors say this is often a decision between doctors and parents.
But Dr. Satyanarayan Hegde, a pediatric pulmonologist at Access Pediatric in Florida, said that if a child had mild illness but was doing well, he would probably choose to “wait and see” rather than operate.
He told DailyMail.com: ‘If I do an examination and find subglottic stenosis but the child is doing well, I might decide to wait and see.
‘Whether surgery is required depends on clinical judgment and what the parents want. Some parents want surgery, but others want to avoid it.”
As children grow during the first six to seven years of their lives, their airways widen, which can help minimize the symptoms the condition causes.
Dr. However, Jonathan Ida, a pediatric otolaryngologist at Northwestern University in Chicago, disagreed and said he would aim for surgery in most patients with subglottic stenosis.
He told DailyMail.com: ‘If I was told there was some degree of subglottic stenosis I would want to evaluate this visually via airway endoscopy.
‘Little children are very resilient and we are often surprised by the visual barriers we encounter during examinations compared to how well they are breathing.’
Research shows that surgeries to treat subglottic stenosis have a mortality rate of less than five percent. It is not clear what percentage of pediatric patients die if subglottic stenosis is left untreated.
According to a 2012 study in JAMAthe success rate for dilation procedures for subglottic stenosis in children – which Carlos received – is approximately 70 percent.
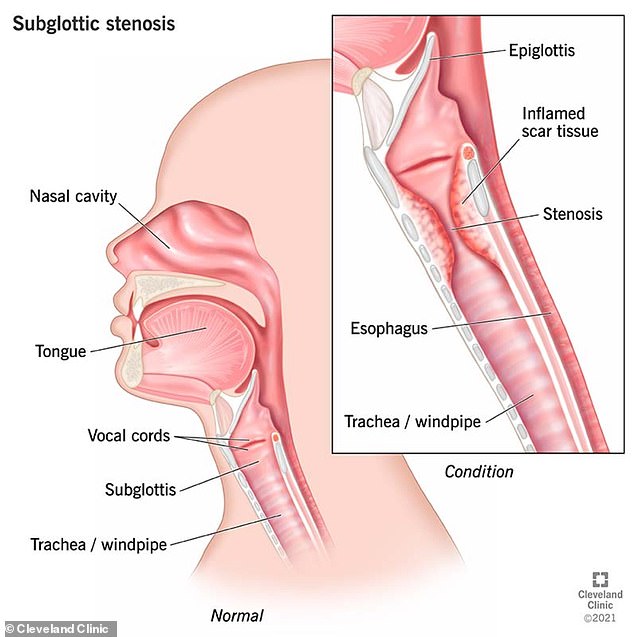
The above image from the Cleveland Clinic shows a normal airway (head) and then one with subglottic stenosis (inset)
Dr. Ida added, “Generally speaking, most people who delay eventually get the intervention for subglottic stenosis.
‘In medicine we talk about the ABCs, the first three things needed to save a life. The first is the airway.”
He explained that surgery is often recommended because if the stenosis persists, it increases the risk of complications later in life if someone needs to be intubated for a condition such as pneumonia.
He also said it was easier to treat earlier in life, when the patient was young.
Warning signs of subglottic stenosis in babies include stridor, a high-pitched whistling sound when a baby inhales or exhales, and recurrent respiratory infections.
Young children who have the condition may also experience a cough that doesn’t go away and shortness of breath.
Treatment options include an endoscopic dilation, a type of minimally invasive surgery in which surgeons split the front and back of the narrowed area in the trachea and insert a small balloon into it to stretch it and open up a larger area.
With a baby it is common to have to do this several times as the area may close again during the healing process.
In some cases, surgeons may perform a cricotracheal resection, or remove the narrowed portion of the airway just below the voice box.
