Breakthrough now that type 1 diabetes in women is being cured for the first time in the world using stem cells
A woman in China’s Type 1 diabetes has been reversed thanks to a new treatment that re-edits cells from the patient’s own body.
The breakthrough treatment converted these cells into personalized stem cells that were then used to grow clusters of fresh ‘islets’: hormone-producing cells in the pancreas and liver that help regulate sugars in the body.
“I can eat sugar now,” said the 25-year-old, who lives in the city of Tianjing, where researchers say her body has been successfully producing its own insulin for more than a year.
The treatment, which outside experts have called stunning and “miraculous,” builds on a related milestone in Shanghai in April.
A woman with type 1 diabetes in China has now proven she can make her own insulin. The breakthrough turned her own extracted cells into personalized stem cells – which were then used to grow clusters of fresh ‘islets’, hormone-producing cells in the pancreas that help regulate sugar
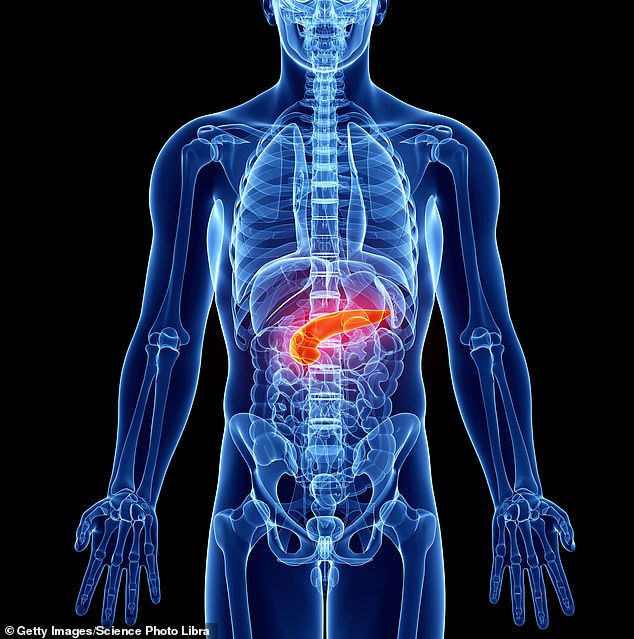
The pancreas is an organ that produces insulin, among other things. Insulin is a natural hormone that our body uses to control the amount of sugar in our bloodstream. People with diabetes have difficulty regulating their blood sugar levels due to pancreatic dysfunction
That April case was different because it involved transplanting stem cells into the liver, while the new method involved transplanting the newly created islets into the patient’s upper abdomen, near her pancreas.
Previous islet transplants in the liver have been more difficult to detect through non-invasive methods such as MRI, experts say, making it more difficult to remove these cell clusters in a worst-case scenario where a patient’s immune system rejects and attacks the transplant.
This new method, in which the islets were inserted just below the abdomen, allowed researchers to monitor the progress of these islets with relative ease via MRI.
“They completely reversed diabetes in the patient, who required significant amounts of insulin beforehand,” transplant surgeon Dr. James Shapiro, who was not involved in the new study, told the journal Natureapproving.
Other independent experts joined Dr. Shapiro, who, as a medical researcher at the University of Alberta in Edmonton, Canada, praised the breakthrough.
“If this is applicable to other patients, it will be great,” diabetes researcher Daisuke Yabe of Japan’s Kyoto University told reporters.
However, some medical professionals were cautious about these results and waited to see if the team’s successful treatment could be reproduced in more patients.
Endocrinologist Dr. Jay Skyler of the University of Miami, who specializes in type 1 diabetes, noted that he would prefer to see if this 25-year-old test patient continues to produce insulin for herself for a total of at least five years before he considers her case truly “cured.” . .’
Health experts have also generally noted that the technique of manufacturing personalized transplants using the recipient’s own cells is currently difficult to scale up cost-effectively – meaning the price tag for this diabetes treatment could be staggeringly high at first.
The medical researchers from Nankai University and Peking University in China behind this new study noted that their test patient was already taking immunosuppressive medications for a liver disease.
Therefore, it remains unclear whether other patients’ bodies might reject a transplant of similar islets derived from their own personally extracted cells.
The June 2023 operation, as the team published in the news Cell on Wednesday, Nam less than half an hour.
‘The patient achieved durable insulin independence from 75 days post-transplant,” as the team from Nankai and Peking University wrote in Cell.

People with diabetes often use blood sugar meters, like this one pictured, to determine how much sugar is currently circulating in their bloodstream. This helps them decide what to eat and when to use insulin to best manage their disease.
By the fourth month after her transplant, the 25-year-old patient’s total time in the desired or target blood sugar range increased from 43.18 percent to 96.21 percent.
Her so-called ‘time-in-target glycemic range’ has since been above 98 percent, the researchers report.
Medical experts have hoped that these types of transplants – which subtly direct the patient’s extracted cells into stem cells and are then used to grow more specialized cells for transplantation back into the patient – would be less prone to rejection by the body.
The hope is that this method will negate the need for immunosuppressants, which help prevent transplant rejection at the expense of a person’s entire immune system.
Several groups, including private pharmaceutical companies, have begun testing their own islet cell transplant treatments, also made using donor stem cells.
Vertex Pharmaceuticals in Boston, Massachusetts, with the help of Dr. Shapiro, has started a trial with a patient who also has type 1 diabetes but is not prescribed immunosuppressant treatment.
“That process is still ongoing,” said Dr. Shapiro.
