America’s early-onset colon cancer death spots revealed.. is YOUR neighborhood one of them?
A study finds that young Americans living in impoverished rural areas are at the highest risk of dying from colon cancer.
Doctors in the US already struggle to detect colon cancer in young people, who are generally not at risk of developing the disease.
But in rural and poor areas the problem is even greater. There, residents have fewer doctors, longer waiting times and more unhealthy lifestyles. All of this increases the risk of cancer.
In the new study, researchers from Augusta University in Georgia looked at nearly 60,000 patients with early-onset colorectal cancer, meaning they were younger than 50 years old.
By comparing federal data on cancer and poverty, the team found that Americans between the ages of 20 and 49 were up to 1.5 times more likely to die from colon cancer if they lived in poor rural areas than those in wealthier urban areas.
Other recent research has found that the disease is more likely to be detected earlier in people living in wealthier, more densely populated areas, making it easier to treat.
With these findings in mind, DailyMail.com has compiled interactive data on colorectal cancer rates among young people in the US, broken down by state and county. However, the county data is limited.
The maps show that young people in states such as Kentucky, West Virginia and Louisiana recorded the most cases of early-onset colorectal cancer. And rural counties in Florida, Arkansas and West Virginia had the highest incidences.
Meanwhile, counties in states like California, New York and the Northeast Coast, where incomes tend to be higher, recorded lower rates of youth-onset colorectal cancer.
It is thought that this form of cancer is strongly influenced by diet, alcohol consumption and a sedentary lifestyle.
Rural areas also tend to suffer from food deserts, resulting in a shortage of fruits, vegetables and fiber-rich foods, which have been shown to reduce obesity and the risk of colon cancer.
The study, which was published on Wednesday JAMA Network Openedanalyzed cancer incidence data from 2006 to 2015 from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database.
The team tracked rates and deaths from colorectal cancer in 58,200 patients aged 20 to 49.
About 43 percent of patients were between 40 and 49 years old, and 53 percent were male.
In addition, one in five people live in rural areas where persistent poverty is prevalent, according to USDA data, putting them at greater risk of developing the disease or not having it detected early.
The team found that the five-year survival rate among young colorectal cancer patients was highest for patients in urban, non-poor areas, at 72 percent.
Meanwhile, in impoverished urban and rural areas, the rate dropped to 67 percent.
And for the youngest group of patients, between 20 and 29 years old, in rural areas with high levels of poverty, the survival rate dropped to 64 percent.
The researchers found that young colorectal cancer patients “who lived in rural areas alone had a 1.1- to 1.4-fold increased risk of dying from colorectal cancer overall compared with patients who did not live in rural areas.”
Patients living in both rural and poor areas were up to one and a half times more likely to die from colon cancer than patients living in urban areas.
While the researchers didn’t name specific locations, federal data shed light on the areas at greatest risk.

Jill MacDonald (left) is a stage four colorectal cancer patient living in Missouri, where one in three residents lives in rural areas. Dr. Dan Bockmann lived in Texas when he was diagnosed, where one in six residents lives in rural areas
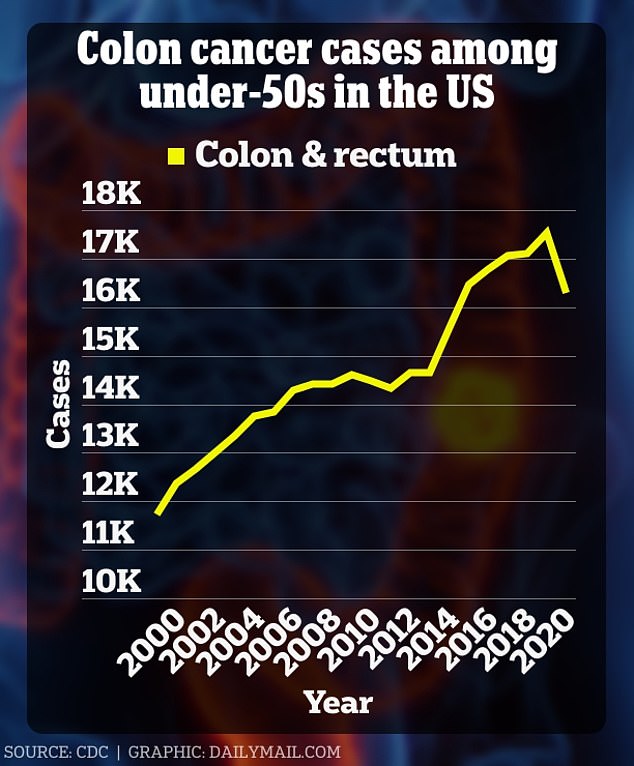
The graph above shows that the number of cases of bowel cancer among the over-50s has increased by more than 5,500 in 20 years. In 2020 there was a decrease, because the Covid pandemic caused fewer people to come forward for screenings.
Based on the most recent county-by-county data from the NCI, Union County in Florida had the highest incidence of young-onset colorectal cancer, with 32 cases per 100,000 residents under 50.
A separate analysis found that the rural region southwest of Jacksonville also tops the list for the most cancers that develop at a young age.
The rural area has a population of only 15,000 and historically tops the list of countries with the highest incidence of lung, oral and skin cancers.
Health officials believe this is due to the area’s high smoking rate and lack of health care funding, as well as one in six residents living in poverty.
USDA data shows the median household income in the area is about $55,000, about a quarter lower than the national average of $75,000.
Life expectancy in the region is also just 67 years, well below the national average of 76 years, according to American News and World Report.
Ouachita County, Arkansas, had the second-highest rate of young-onset colorectal cancer, with 25 cases per 100,000 residents. The southwestern county has just 22,000 residents, and the median household income is about $44,000, about 40 percent below the national average, according to USDA data.
Mingo County, West Virginia, also had 25 cases per 100,000 people. Also home to about 22,000 residents, the area’s household income is about $35,000, less than half the national average.
In terms of state data, West Virginia also tops the list for cases of young-onset colorectal cancer, with 11 cases per 100,000 people.
Experts say the Mountain State’s high rates may be due to its high prevalence of obesity, which can lead to excessive inflammation that promotes the growth of cancer cells.
West Virginia also has the highest smoking rate in the country. Smoking is a known risk factor for colorectal cancer because it disrupts the gut flora.
Arlington County, Virginia, had the lowest rate of young-onset colorectal cancer at 4.9 cases per 100,000 people. According to USDA data, the metro area’s household income is $128,000, nearly 40 percent above the national average.
