British doctors are on alert over the spread of a deadly new variant of the mpoxvirus – after the WHO declared a global health emergency following the outbreak in Africa
Health authorities have ordered doctors to be on the alert for cases of mpox as a deadly variant has been confirmed to have reached Europe.
The World Health Organization has declared a global public health emergency – the highest level of alert – after an outbreak in Africa.
The first case outside the continent was identified in Sweden, leading the European Centre for Disease Prevention and Control to raise the risk level.
Experts say the new variant is “more serious” and has a “higher mortality rate” than the variant that caused panic in 2022. According to the UK’s Health Security Agency, no cases have been identified yet and the risk to the population is “low”.
Rapid tests are being made available and GPs and hospitals have been told to isolate people with symptoms. The government is said to have enough vaccines and treatments to combat an outbreak.
Christian Musema, a laboratory nurse, takes a sample from a child suspected of having Mpox at the treatment center in Munigi, Democratic Republic of Congo

The first case outside the continent was discovered in Sweden, prompting the European Centre for Disease Prevention and Control to raise the risk level. Pictured: Test tubes labelled ‘Monkeypox virus positive and negative’

Swedish State Epidemiologist Magnus Gisslen, Acting Director General of the Public Health Agency Olivia Wigzell and Minister of Social Affairs and Health Jakob Forssmed will give a press conference on August 15 to inform about the mpox situation in Stockholm.
An NHS England spokesman said it was “ready to respond” if the variant, which has already killed 537 people, emerged here.
The deadly variant emerged this month and is crossing national borders. A death rate of 10 percent is reported in children. The variant threatens to decimate the population and authorities are powerless to stop its spread.
Researchers warn that the new variant of the disease, ‘Clade 1b’, has already been able to cross the DRC’s ‘porous’ borders, killing dozens of people in Burundi, South Africa and DR Congo in recent weeks, while many thousands have been displaced by conflict in the region.
Mpox is typically found in Central and East Africa and has been ravaging populations since the early 1970s. Although a vaccine now exists for the disease, uptake has been slow in countries that lack the resources and infrastructure for a coordinated program.
Nearly 100,000 people were infected in 2022 during a global outbreak of the disease, mainly caused by the Clade IIb virus. The variant was less deadly than the emerging Clade Ib variant, but killed about 183 people, the CDC said.
In the United States, a staggering 32,063 cases were reported during that period, with 58 deaths. Significant numbers of cases were reported in North, Central and South America, Europe, Africa, Asia and Australasia.

Christian Musema, a laboratory nurse, takes a sample from a child who has been diagnosed as a suspected case of Mpox

A child with skin lesions receives treatment at the treatment center in Munigi, DRC, on July 19
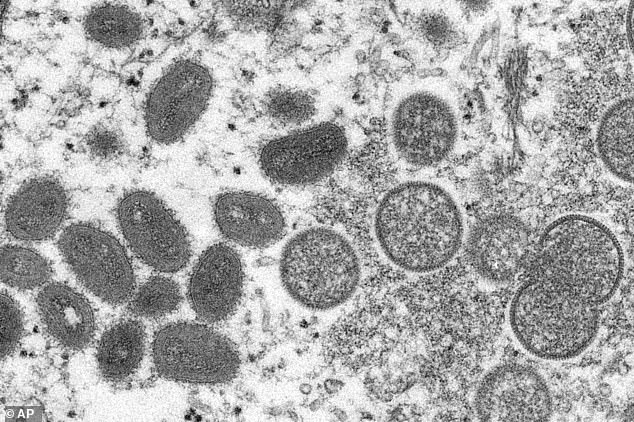
Mpox virions shown under a microscope. Experts warn that the new 1b Clade is harder to detect

A 1997 image shows symptoms of MPOX in a patient in DRC, formerly Zaire
The Africa CDC said earlier that mpox, formerly known as monkeypox, has been detected in 13 countries this year, with more than 96% of all cases and deaths in Congo. Cases are up 160% and deaths are up 19% compared to the same period last year.
So far, there have been more than 14,000 cases and 524 people have died.
Experts monitoring recent trends now warn that a deadlier variant is increasingly crossing borders, with a fatality rate of five percent in adults and ten percent in children.
While the 2022 variant was largely caused by sexual contact between men, the Clade Ib variant appears to be transmissible through close non-sexual contact and exacerbated by heterosexual sexual contact, “particularly among sex workers, who account for about 30 percent of recorded cases,” according to The Economist.
Authorities in the Democratic Republic of Congo approved MPOX vaccines in June in a desperate bid to contain the outbreak, which has killed more than 1,000 out of 20,000 people in the past year. But many fear that affected countries lack the resources to effectively stop the spread.
Zeil Rosenberg, MD, executive vice president of Tonix Pharmaceuticals, a company currently developing an mpox vaccine, told MailOnline earlier this month that the disease is now spreading to areas where it was not previously endemic.
“The Democratic Republic of Congo (DRC) continues to be at the centre of an unchecked explosion of cases, with 11,000 cases reported this year alone and showing no signs of abating,” he warned.
‘There are a number of challenges in controlling this outbreak,’ Brian Labus, assistant professor in the Department of Epidemiology and Biostatistics at the University of Nevada Las Vegas, told MailOnline.
“We have seen spread in camps for internally displaced people, where high population densities increase the risk of spreading infectious diseases.”
He warned that the virus has mutated and is now spreading more easily between people.
‘Although we can prevent the disease with vaccines, these are currently not available in the affected areas.
‘When you add these issues to the daily challenges of fighting diseases in remote, resource-poor areas, it has proven very difficult to control the outbreak.’
Michael Marks, professor of medicine at the London School of Hygiene and Tropical Medicine, said declaring the mpox outbreak in Africa an emergency is justified if it can lead to more support to contain the outbreak.
“It is a failure of the global community that the situation had to get to this point to release the necessary resources,” he said.
According to officials at the Africa CDC, nearly 70% of cases in Congo involve children under the age of 15. They also account for 85% of deaths.
Jacques Alonda, an epidemiologist working in Congo with international charities, said he and other experts were particularly concerned about the spread of mpox in refugee camps in the conflict-torn east of the country.
“The worst case I have ever seen was a six-week-old baby who was only two weeks old when he was given mpox,” Alonda said, adding that the baby has been in their care for a month.
‘He became infected because the hospital was overcrowded and he and his mother had to share a room with someone else who had the virus, but it had not been confirmed.’
