Blood test for male infertility could be on the horizon: AI can screen men with 74% accuracy – with no semen needed
Scientists say GPs will soon be able to perform a rapid fertility test for men that requires only a blood sample.
The test, developed by Japanese researchers, uses artificial intelligence (AI) to look for hormones in a blood sample that could indicate low sperm counts in semen.
According to the experts, the AI model has 74 percent accuracy in detecting low sperm counts.
But it is 100 percent accurate in predicting non-obstructive azoospermia — a severe lack of sperm in the ejaculate and a primary cause of infertility.
In the near future, men will be able to get a small prick in their finger for a blood sample. This blood sample can be sent for analysis to determine the risk of infertility.
In the future, AI blood sample analysis could become an established screening method for male infertility, replacing sperm tests (file image)
The test is being developed by a group led by Professor Hideyuki Kobayashi of the Department of Urology, Toho University School of Medicine in Tokyo, Japan.
‘Normally the first step in diagnosing male infertility is to do a semen analysis and if any abnormalities are found then a hormone test is done,’ he told MailOnline.
‘What is unique about this study is that it is groundbreaking, because the risk of male infertility is determined based on a hormone test, rather than a sperm test.’
‘Semen testing is a simple test, but it is not an adequate way to detect male infertility. Only fertility centres have the space for ejaculation and the specialised equipment to perform the test,’ says Professor Kobayashi.
‘There are also men who are socially or religiously unable to ejaculate through masturbation.’
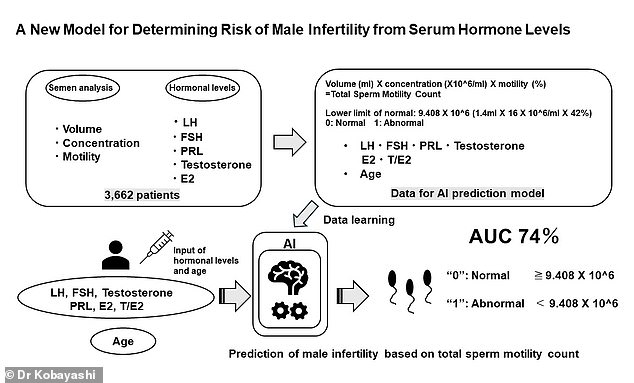
This graphical abstract explains the new model for determining male infertility risk based on blood hormone levels
Semen analysis is considered essential for the diagnosis of male infertility, but is not readily offered in medical institutions other than those specializing in infertility treatment.
“Fertility specialists assume that the first step in diagnosing male infertility is to perform a semen analysis,” adds Professor Kobayashi.
‘This is the world’s first AI prediction that determines the risk of male infertility without a sperm test.’
He trained his AI computer prediction model on data from 3,662 men who underwent sperm and hormone testing for male infertility between 2011 and 2020.
The sperm volume and sperm concentration of each male semen sample were measured.
Sperm motility was also measured: the ability of sperm to move efficiently, which is of course related to the fertilization of an egg.
The blood samples also measured several hormones that have been associated with high or low sperm counts in semen, including testosterone, follicle-stimulating hormone (FSH), prolactin (PRL) and estradiol (E2).

According to the World Health Organization, about half of all infertility is due to men. Semen analysis is considered essential for diagnosing male infertility, but is not readily available in medical facilities other than those specializing in infertility treatment (file photo)
The AI model was then validated using data from 2021 and 2022, for which both sperm and hormone tests were available.
Using data from 188 patients in 2021, accuracy was approximately 58 percent, while using data from 166 patients in 2022, accuracy was approximately 68 percent.
However, non-obstructive azoospermia – defined as the absence of sperm in the ejaculate – could be predicted with 100 percent accuracy in both 2021 and 2022.
The researchers report that the model had an accuracy rate of 74 percent based on data from 3,662 patients.
“This AI prediction model is only intended as a primary screening step prior to sperm testing,” said Professor Kobayashi.
‘While it is not a substitute for sperm testing, it can easily be performed in settings other than those specializing in infertility treatment.
‘If the prediction model detects abnormal values, because patients may have non-obstructive azoospermia, this should be a reason for them to be examined at a specialized fertility clinic and receive appropriate treatment.’
Professor Kobayashi said his team has already granted a patent and is working with a company called Clear Tact Inc to bring the product to market.
‘Our goal is to have it on the market within five years and I think the market will start in Japan,’ he told MailOnline.
The full results were published in the British scientific journal Scientific Reports.
