GPs threaten ‘catastrophic’ strikes that could halve daily appointments
GPs have threatened to bring the NHS to a ‘standstill’ with unprecedented strikes, including cutting the number of appointments by a third.
The British Medical Association is calling on GPs to support the revolution. It is the first time in 60 years. Voting closes at 12 noon today.
Patient groups last night branded the measure “selfish” and warned GPs they risk harming people in need of care – and losing public support.
A cap on the number of appointments could be ‘catastrophic’, an NHS director has said.
It is feared that as many as 3 million GP appointments a month could disappear if all GPs bow to the BMA’s demands to reduce the number to just 25 a day. Some are now doing 50, while the average is 37.
It is feared that around 3 million GP visits per month could disappear if all GPs comply with the BMA’s demands to reduce the number of visits to just 25 per day.

BMA representatives previously met with Health Minister Wes Streeting (pictured)
The action is scheduled to begin next Thursday and last ‘for months’.
The union says funding for GPs is under pressure and the terms of a new NHS contract mean “many practices will struggle to remain financially viable”.
But GPs who run their own practices, who make up the majority of GPs, earn an average of £153,400 a year, despite the fact that only one in three works full-time.
If GPs support the vote, they can participate in nine forms of protest. One of these is setting a maximum number of daily ‘patient contacts’.
This includes face-to-face appointments, remote consultations and online messages.
According to the BMA, practices must limit this number to 25 per GP per day. That is a third less than the current typical workload.
Dr Katie Bramall-Stainer, chair of the BMA’s general practice committee, said GPs would not ‘strike’ but would engage in ‘collective, premeditated, disruptive action’.

GP employment data for May 2023 shows there are 27,200 fully qualified GPs in England. This is down from 27,627 a year earlier. The number of GPs peaked at 29,537 in March 2016
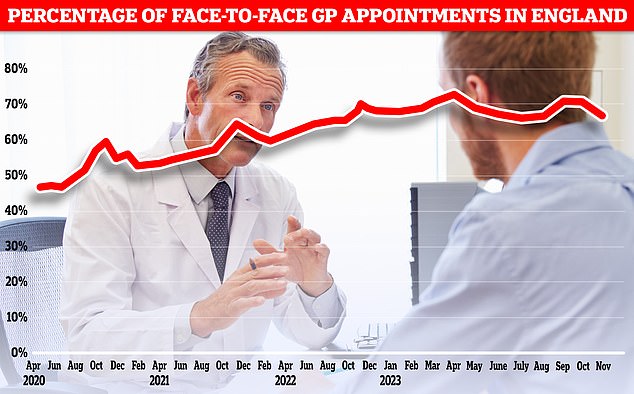
Separate figures show that just 68.3 percent of appointments in November were face-to-face, down from around 80 percent before the pandemic. It is also the lowest figure so far this year
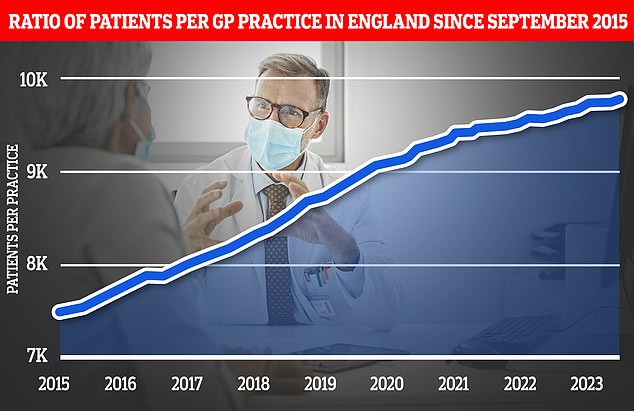
The graph shows the ratio of GP patients to practices since 2015, with an average of 9,755 patients per practice in May 2023.
She said the action was aimed at hitting NHS England and the Department of Health and Social Care, not patients.
Dennis Reed, director of Silver Voices, which campaigns for people over 60, told the Mail: ‘Our members, who already struggle to get doctor appointments on time, will be appalled and angry at this premature action by GPs.
‘Since no disruptive action was taken in the last five years of the previous government, despite broken promises about recruiting more doctors, they are not giving any chance to negotiations with the new government.
“It is laughable to say the action is aimed at NHS England when it is patients who are suffering from further restrictions on appointments.
‘The proposed measure will only lead to more patients overwhelming emergency departments.
‘Some older patients are sent away by their GP and go home. They then run the risk of their symptoms getting worse.’
He added: ‘Silver Voices supports the call for more resources for primary care and is sensitive to the workload of GPs, but this self-serving action over the detailed terms of generous contracts risks losing public support for their cause.
“The way to solve these problems is through mature negotiations, not by waving weapons.”
Matthew Taylor, chief executive of the NHS Confederation, told the Guardian: ‘If all GPs were to implement the patient cap, it could have disastrous consequences for the whole health system.
‘GP practices are now treating more patients than before the Covid pandemic. If they are treating fewer patients, this will put more pressure on other services, including emergency care.’
The vote, which started on 17 June, could also lead to GPs stopping work for which they do not have a formal contract, refusing to participate in local data-sharing agreements and flouting NHS ‘rationing’ restrictions on medicines.
On Monday, NHS England urged local health leaders to prepare for a “reasonable worst-case scenario” of GP strikes, warning that it could have implications for the “whole system”, including A&E.
Professor Helen Stokes-Lampard, former chair of the Royal College of GPs, told NHS England’s board meeting on Thursday that the NHS was “already beginning to experience strains” as GP practices “pull back” from discretionary work.
GPs have not taken action since 1964, when GPs submitted their collective undated resignations to the Wilson government.
But the BMA has recently led strikes by junior doctors and specialists, making it difficult to clear waiting lists that have built up during the Covid-19 pandemic.
The BMA said the new GP contract, which sees funding for services increased by 1.9 per cent for 2024/25, means many practices will struggle to remain financially viable.
But official figures from NHS Digital show that GP practices’ income (which comes from the profits of their practices) has risen by 31 per cent in recent years.
Dr Bramall-Stainer said the action was designed to be ‘simple, sustainable and effective’, adding: ‘If it is done effectively, collectively and well, it will bring the NHS to a standstill very quickly – but not for patients, not for all of the NHS administration, the policymakers who have made these decisions that do not help patients.’
GPs launched a formal dispute over the issue in April after a union referendum found 99 percent of the 19,000 GPs had rejected the contract.
Dr Bramall-Stainer said: ‘We don’t want to put patients in the middle like pigs – we live in our communities with our patients, there are no barriers between us.
‘We get a lot of criticism about the failures of the NHS and we agree with our patients and it’s quite tiring. The last thing we want to do is turn patients against us.
“I don’t think patients will really notice much of a difference. And that’s the plan.”
Dr Bramall-Stainer met with Health Minister Wes Streeting on July 18 and union leaders hope such talks will continue.
Earlier this month, she presented a number of requests to the government, including a new Charter for GPs, a ‘minimum investment standard’ for GP practices, a request to realise ‘reinvestments in real terms’ in GP practices and a call for ‘GP-patient ratios’.
Mr Streeting’s first official visit in his new role was to a GP surgery in London on 8 July, where he promised to ‘bring back the GP’ and ‘fix the front door of the NHS’.
A Department of Health and Social Care spokesperson said: ‘The Secretary of State for Health and Social Care has met with the Chair of the BMA’s GP Committee to discuss their priorities ahead of the close of voting on 29 July.
‘However, it is important that we consider all eventualities so that patients remain safe.’
NHS England said: ‘We continue to work with GPs, the BMA and the government to help prevent potential measures, but in the meantime the NHS has a duty to plan for potential disruption and ensure services continue to be delivered for patients. That’s why we continue to work with local systems to help them plan for the eventuality that collective measures are taken.’
