‘Groundbreaking’ DIY smear tests will soon be rolled out across the NHS after major study shows they significantly increase uptake of cervical cancer screening
Britain’s National Health Service (NHS) is to introduce home swab tests after they were found to significantly increase screening uptake and potentially save thousands of lives.
The self-test kits are expected to revolutionise cervical cancer diagnosis after the largest study to date found they could reach an extra million women every three years.
The test can be sent by post or collected from a GP surgery, allowing women to collect samples in the comfort of their own home.
Health officials said the “groundbreaking” new method would likely save the lives of thousands of women who never got screened or got screened too late.
King’s College London’s first national screening programme found that it could help researchers reach an additional 400,000 women in England each year.
Cervical cancer screening participation has declined over the past two decades, with almost a third of women in England not having their final test.
Self-test kits like this one (pictured) are expected to ‘revolutionize’ cervical cancer diagnosis

Many younger women in particular do not respond to invitations because they are afraid of the test and feel uncomfortable or ashamed by it.
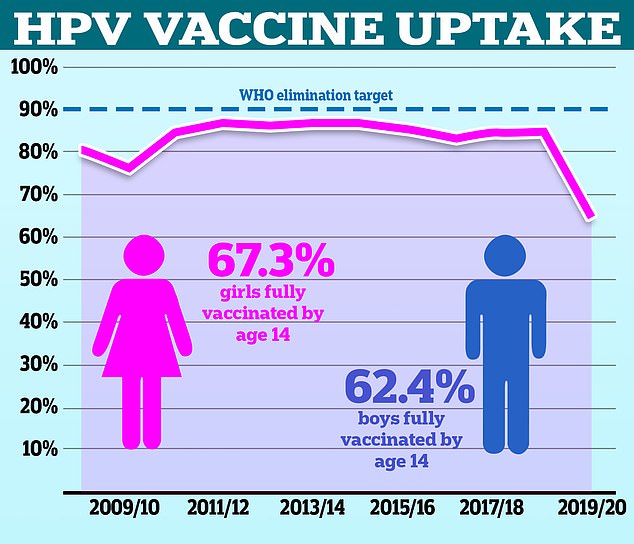
Only 67.2 per cent of girls were fully vaccinated in 2021/22, down from a peak of 86.7 per cent in 2013/14. About 62.4 per cent of boys offered the jab through the NHS since 2019 were vaccinated in the most recent school year, NHS data shows
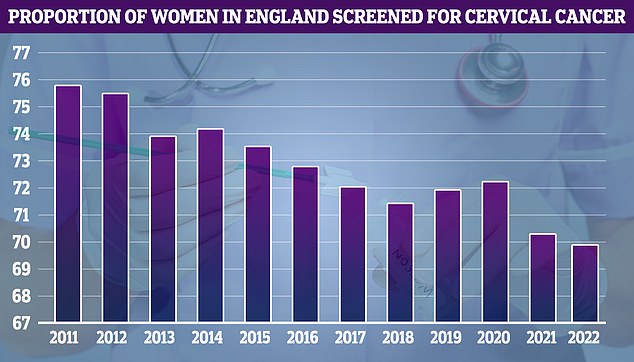
NHS cervical screening data going back to 2011 shows that participation was highest that year (75.7 per cent) and has declined over time
Experts say it could help ‘make cervical cancer a rare disease in the UK’.
Cervical cancer screening participation has declined over the past two decades, with almost a third of women in England not having their final test.
Many younger women in particular do not accept invitations. They state as reasons that they are afraid of the pain that the test entails, are ashamed and that suitable appointments are not possible.
In the new study, more than 27,000 YouScreen kits were distributed by 133 GP practices in north and east London to women aged 25 to 64 who were overdue for their screening, either through their GP or by post.
The swab is easy to use and detects the human papillomavirus (HPV), a group of viruses responsible for almost all cases of cervical cancer.
Women used a vaginal swab – a type of long cotton bud – to collect their sample at home or in their GP’s office.
Of the 10,849 women who were offered a pack when they discussed something else with their GP, 85 percent accepted the offer and 6,061 (56 percent) provided a self-sample.
People who took the test at home could send their test kit to a laboratory for free.
Half (52 percent) of all women who had done a self-examination were at least two years overdue for screening. This was also true for women who had never been screened before.
According to the researchers, routine rollout of the kits in England could increase screening coverage from 70 to 77 percent.
Lead researcher Dr Anita Lim from King’s College London said: ‘Self-sampling is seen as a game-changer.
‘It is vital that we make cervical cancer screening easier… to protect more people from this highly preventable cancer.
“The YouScreen study has given us the evidence we need to show that self-screening leads to more women getting screened.”
The NHS invites women for screening every three to five years, depending on their age. If HPV is found, this may be more frequent.
The evidence shows that self-collected tests are as good at detecting pre-cancerous cells as the standard cervical cancer screening test performed by a doctor or nurse.
The Department of Health and Social Care said last night: ‘This trial demonstrates a ground-breaking new way to screen for HPV, which could potentially save thousands of lives.’
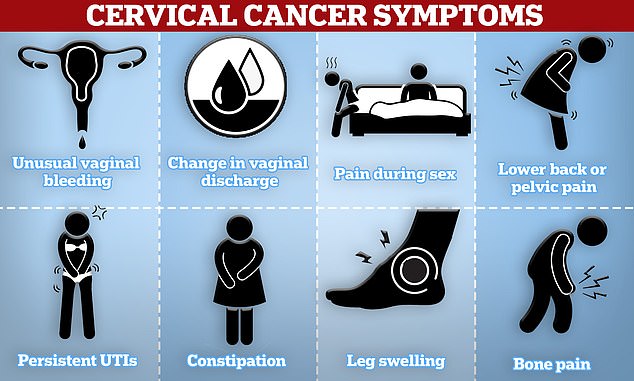
Symptoms of cervical cancer to watch for include unusual vaginal bleeding, pain during sex, and lower back or pelvic pain.
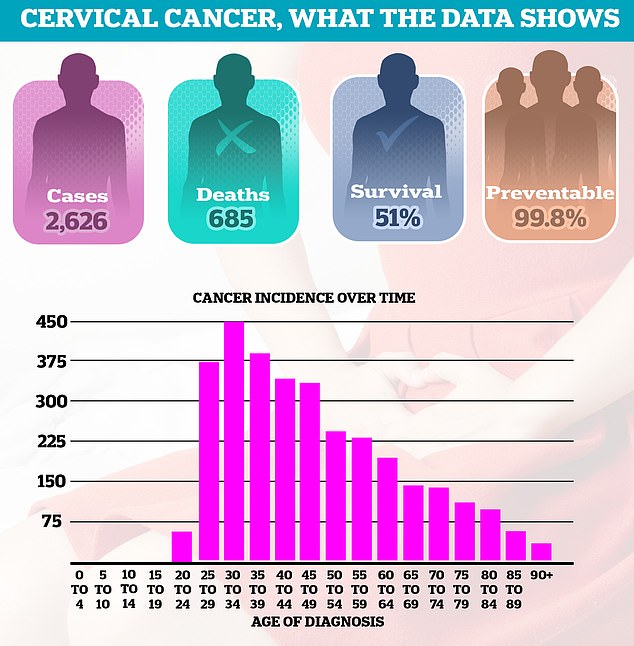
Thousands of women are still diagnosed with cervical cancer each year, leading to 685 deaths in England each year. Around half of women (51 per cent) survive 10 years or more after diagnosis. Diagnoses are most common in women in their 30s.
52 percent of all people who provided a self-sample were at least two years late with screening, including women who had never been screened before

The NHS invites women for screening every three to five years, depending on their age. If HPV is found, this may be more frequent.
In the UK, there are around 3,300 new cases of cervical cancer and 850 deaths each year.
Last night, Professor Peter Sasieni, head of the research group at King’s College London, said: ‘We are well on our way to making cervical cancer a rare disease in the UK.
‘YouScreen has shown that this simple test is popular with both women and GP practices and that it could increase screening participation by over a million people in three years.’
According to the study published in the journal eClinicalMedicine, other countries, such as the Netherlands, Australia, Denmark and Sweden, have already introduced the self-test kits.
Deborah Tomalin, NHS director of screening and vaccination, said: “The NHS will now work with the UK National Screening Committee to explore the feasibility of a wider rollout of this across England.”
