New test can predict whether prostate cancer will return… and could save thousands of lives, experts claim
Scientists can predict the chance of prostate cancer returning up to ten years earlier than it actually does, which could greatly increase survival chances.
In approximately half of men who develop locally advanced prostate cancer, the disease will return, often with a poor prognosis.
But a new test – which combines genomic sequencing and artificial intelligence (AI) – could identify those most at risk at first diagnosis.
If doctors know who is more likely to have recurrences, they can treat these patients more effectively, giving them the best chance of preventing the cancer from coming back.
Experts believe that after larger-scale testing, the drug could be widely used within three years and save the lives of thousands of men in the future.
A new test – combining genomic sequencing and artificial intelligence (AI) – can identify men at highest risk of prostate cancer recurrence when first diagnosed
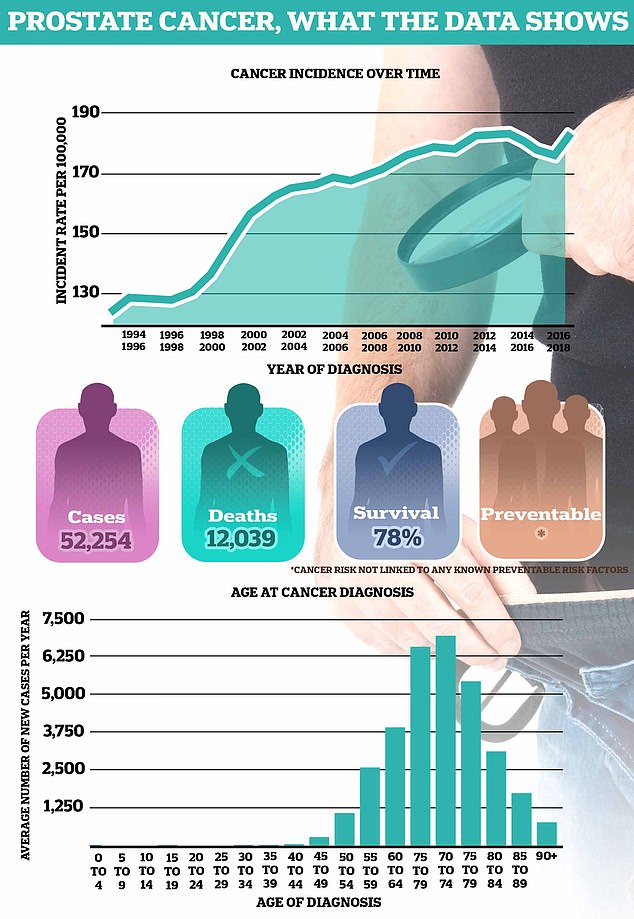
On average, more than 52,000 men in the UK are diagnosed with prostate cancer each year, making it the most common cancer in men. Around 12,000 men die from the disease each year — the equivalent of one every 45 minutes
Prostate cancer is the most common cancer in men and the second deadliest, killing around 12,000 men each year in the UK.
There is no test reliable enough to enable a national screening program to detect cases early, limiting the chances of survival.
The disease can be difficult to treat because of its great heterogeneity: there are significant differences between the cancer cells in each tumor and from patient to patient.
Often the condition develops in more than one place in the prostate, with two or more tumors developing, making it difficult for doctors to determine the best treatment.
This can vary from a wait-and-see approach to radiotherapy, hormone therapy, surgery or a combination of treatments.
Researchers from the Institute of Cancer Research in London and The Royal Marsden NHS Foundation Trust have developed an AI tool to assess biopsies taken at the time of diagnosis.
They used it to analyze 1,923 samples from 250 patients from a previous clinical trial, focusing on the spatial tissue structure of the cancer biopsies.
They also used a specially developed AI technique to perform Gleason grading: a scoring system that gives cancerous tissue a grade from one to five based on the pattern of cells.
At the same time, the researchers assessed the genetic differences between the cells within individual tumors, using 642 biopsy samples from 114 participants in the same radiation therapy study.
This allowed scientists to simultaneously assess information about the genomics and morphology of the cells, to see how both influenced the chance of recurrence.
Because the study was long-term, they were able to analyze it in comparison to the outcomes of the patients over a period of more than ten years. This is of great importance in prostate cancer, since this form of cancer can grow slowly.
They found that the greater the genetic difference between cells – and the greater the difference between the shape, size and structure of the cancer cells in a tumor – the greater the chance of relapse.
Professor David Dearnaley, Emeritus Professor at the ICR and retired clinical oncologist at The Royal Marsden, said the findings could have a significant impact on patients who traditionally have a poor prognosis.
“It’s potentially very exciting for the future,” he said.
‘We were able to determine that the 20 percent of patients who did the worst, did really badly compared to the rest. That’s exciting because it means you’ve potentially defined the group where you can intensify treatment.
‘There are currently several possible treatment methods. If we can improve the treatment methods, we can also increase the chances of recovery.
‘Until now, we have not been able to identify patients with the highest risk of cancer recurrence, but our new analyses could change this. They will enable us to predict much better whether the cancer will return.’
The study, which will be published later today (Friday) in Nature, found that the more differences there were between the shape, size and structure of cells, the more likely the cancer was to adapt and survive. This ‘evolvability’ was therefore a strong predictor of recurrence.
Researchers were also able to identify a subgroup of patients whose disease returned twice as quickly as the rest of the patients.
In the UK, more than 52,000 men are diagnosed with prostate cancer each year, compared to 299,000 in the US.
There was also a link between the loss of a specific chromosome and a reduced presence of immune cells in the tumor. This could affect the response to certain treatments and could determine clinical decisions.
Andrea Sottoriva, a professor of cancer genomics and evolution at the ICR at the time of the research and now based in Milan, Italy, said the findings “have never been shown before.”
He added: ‘By applying a computational approach to multiple datasets, we have been able to unravel some of the dynamics of cancer progression and treatment resistance.
‘This type of research is crucial to gain more insight into how and when we should treat cancer, including prostate cancer.’
This comes as a ground-breaking study into prostate cancer is being carried out in the UK, likely to be followed by a national screening programme.
Transform will test the effectiveness of diagnostic techniques, including MRIs, against the current standard blood test for prostate-specific antigen (PSA).
The Mail has been campaigning for better outcomes in prostate cancer for more than two decades.
Researchers will now conduct tests on a larger, more diverse group of men, but expect this type of technology to become routine in the future.
Dr Hayley Luxton, Senior Research Impact & Intelligence Manager at Prostate Cancer UK, said: ‘It’s devastating to get the news that your prostate cancer has come back after being given the ‘all clear’ advice. Because every man’s cancer is unique, it’s a huge challenge for doctors to predict whether this will happen and to come up with the best treatment plan to prevent it.
‘This project is exciting because the researchers have combined evolutionary studies and AI to develop innovative tools that can be used to identify men whose prostate cancer is likely to return sooner rather than later. This will allow doctors to combat this by providing these men with the most effective, tailored treatment.’
Ends
