‘Killer’ antibiotic STILL prescribed to 15 million Americans a year: Singer Bobby Caldwell’s widow reveals how pills he was prescribed for colds left him paralyzed and suffered ‘excruciating’ nerve damage – leading to his untimely death
The widow of legendary singer Bobby Caldwell has revealed his final years of hellish battles caused by a common antibiotic that were at the center of multi-million dollar lawsuits.
The star was prescribed fluoroquinolone to treat a cold in 2017 but was bedridden within a week. It ravaged his body and caused ‘excruciating’ nerve damage, setting him on a fatal course that ultimately led to him dying from heart disease last year at the age of 71.
‘It was so wild and sudden. It just devastated my husband,” Mary Caldwell told DailyMail.com.
For much of his final years, the confident artist she knew and loved would just “sit and cry” because of the excruciating pain he felt.
Mary tries to raise awareness so others don’t have to suffer like Bobby did, but the drug is still prescribed to tens of millions of Americans every year.
Last week it was reported that a mother, who had been prescribed a drug from the same family of antibiotics to treat her urinary tract infection, used to be was unable to walk after having a similar reaction.
Happily in love: Bobby and Mary Caldwell on their wedding day in 2004


Bobby suffered devastating effects from a fluoroquinolone antibiotic he was prescribed. “The pain started at the bottom of his feet and ankles, and as time went on the pain continued to rise, all the way down to his knees, eventually affecting his hands,” his wife told DailyMail.com
Bobby’s ordeal began on January 13, 2017, a date his wife will never forget: It was her birthday.
Bobby had a ‘nasty’ runny nose and cough and was prescribed cough syrup and Levaquin – a brand of levofloxacin, a type of fluoroquinolone used to treat bacterial infections.
He took seven pills over the course of seven days.
“I didn’t think anything of it,” Mrs. Caldwell said. Just a week later, Bobby couldn’t get out of bed.
“Maria, I can’t get up. My ankles are killing me,” he told his wife.

Bobby’s foot. The drug tore both his Achilles tendons
His ankles started to swell. “It was incredible,” Ms. Caldwell said. “It dawned on me (that it might be the medicine).”
Mrs. Caldwell picked up the bottle and Googled it. “It sent a chill down my spine because I started seeing horror stories and law firms,” she said.
It turned out that the drug had ruptured both of Bobby’s Achilles tendons over the course of the week.
Dr. Mark Ghalili, a board-certified physician from Los Angeles, California, told Daily Mail.com that the drug “causes disruption in the production of collagen.”
“If you can’t produce collagen, you end up with very weak and fragile tendons,” he said.
In 2008, the first black box label was added to fluoroquinolones to warn patients of the increased risk of tendon rupture and tendonitis (inflamed tendons).
The problem affects up to one in 250 patients, but the older the patient, the greater the risk of the damage causing wider health problems.
Doctors don’t learn about it in medical school, Dr. Ghalili said, so they don’t inform their patients about it.
“The pain started at the bottom of his feet and ankles, and as time went on the pain continued to rise, all the way down to his knees, eventually affecting his hands,” Ms Caldwell said.

Bobby and his wife in San Francisco
‘He felt nothing. His fingers were numb. He was in constant terrible pain. He couldn’t sleep much. If he slept for two hours straight, that was a lot.”
“He suffered until the day he died,” Mrs. Caldwell said.
Bobby’s nerve damage was irreversible, so doctors could only offer him pain medication, which didn’t work, his wife said.
The couple sought advice from doctors across America, but “no one could solve it.”
“(Bobby’s Achilles tendon rupture) was horrible, but that wasn’t the worst of it,” his wife said.
The antibiotic had also caused permanent nerve damage, causing Bobby to develop peripheral neuropathy, which caused “relentless, horrific pain”, Ms Caldwell said.
Fluoroquinolones quickly stop the activity of essential enzymes, meaning bacteria cannot multiply.
The drugs only enter cells where nasty bacteria are present. They interfere with the DNA, causing the cells to stop producing enzymes and die.
The medicines work quickly, so side effects can also occur very quickly.
Nerves are covered with endoneurium – a layer of fragile connective tissue composed of collagen fibers.
“When you break down the collagen fibers that protect a nerve, you expose the nerve to oxidative stress and damage,” said Dr. Ghalili.
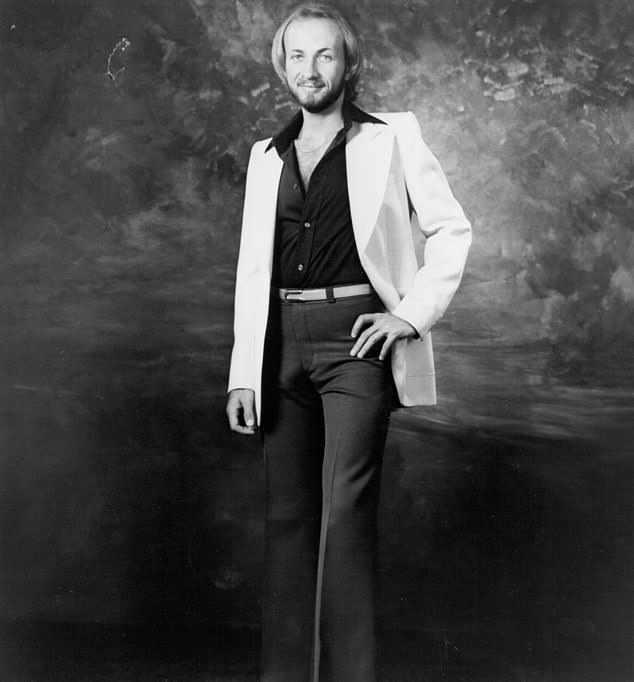
His very first days: Here the artist can be seen in 1970 in a photo of PBR INT
Dr. Ghalili sympathizes with Bobby because of his own brush with death after being prescribed the antibiotic as a young man.
“At my worst, I had called local cemeteries and sent my last wishes to my family,” he told ABC.
Currently, six fluoroquinolones are approved for use in the US: ciprofloxacin, ofloxacin, gemifloxacin, levofloxacin, moxifloxacin, and delafloxacin.
According to CDC figures, approximately 14.8 million people were prescribed these medications in 2022.
Recommended uses include: anthrax, gonorrhea, typhoid fever, complicated bacterial infections and urinary tract infections if other treatments have failed.
The FDA has received reports of hundreds of thousands of serious adverse events related to fluoroquinolones from more than 60,000 patients since the 1980s.
The most common side effects are tendon rupture and neurological and psychiatric symptoms.
The drug is intended as a last resort but is overprescribed by doctors, according to the American Pharmacists Association.

RIP: Mary, whom he married in 2004, wrote on Twitter: ‘Bobby passed away here at home. I held him tight in my arms as he left us. I am forever heartbroken.”
“You are never taught in medical school about the side effects of these drugs,” Dr. Ghalili said.
‘I have spoken to many people who have suffered from it or know someone (who suffers from it). There have been people who have died after two doses,” Ms Caldwell said.
“The other scary part… you could take Cipro or Levaquin and everything would be fine. The next time you take it, all hell will break loose.”
She added: “I’m not saying the medicine doesn’t have a purpose, because it does. If you have anthrax, or if you have a bacterial infection that doesn’t respond to antibiotics, this is the big gun as a last resort.
‘You may still get the side effects, but it could save your life. The problem is that these doctors throw it at people. Oh, do you have a urinary tract infection? Please. Oh, you have some kind of infection. Please. Oh, do you have some kind of infection? Please.
“It’s a drug with a black box warning label, it has a history of lawsuits and FDA warnings here in the United States. I wonder: are the doctors doing their homework?’
Bobby was never informed about the risks of the medication, his wife claimed.
“The man just gave him the recipe. The pharmacy didn’t say anything.’
“If you read the FDA’s black box warning, it says you shouldn’t give this to people over 60 years old. It basically says this is a last resort.”
Bobby was 65 when he got the prescription.
As the nerve damage caused him severe pain and his torn tendons left him bedridden, Bobby was set on a fatal course and eventually died of heart disease.
“He died in my arms,” Mrs. Caldwell said.
‘My message is: look it up, discuss it before you swallow anything. Ask if it has a warning label in the black box,” she said.

Dr. Ghalili became seriously ill and disabled after being prescribed the antibiotic Cipro
“Don’t trust blindly because that’s what we did… You really have to ask questions and do your own research. If they say no, it doesn’t happen. Excuse me, but bulls***. It happens.
“The scary thing is that once it happens, more often than not, if you get affected by it, like Bobby did, there’s no going back,” she added.
In December 2016, Dr. Ghalili had just completed medical school. He had also been prescribed Cipro for an infection.
He was running on the treadmill at the gym when his legs buckled and he lost control of his limbs.
Dr. Ghalili lost the ability to walk and was forced to crawl. “The drug poisoned me,” he said.
Before the incident, Dr. Ghalili had even prescribed the drugs to his own patients.
He turned to alternative therapies, and after six months in a wheelchair, an experimental stem cell infusion helped him walk again.
Dr. Ghalili now works to help patients recover from the devastating effects of receiving antibiotics.
