Memory loss may be REVERSIBLE in up to 10 percent of dementia patients, intriguing study suggests
As many as one in 10 dementia patients could alleviate some of their symptoms by treating an underlying liver problem, an intriguing new study suggests.
One of the most important of the liver Functions include filtering toxins – such as ammonia and manganese – from the blood that can disrupt communication between brain cells.
But if the organ fails, these compounds remain in the blood, in a condition called liver cirrhosis – or liver scarring – and can cause dementia-like symptoms.
Researchers from Virginia Commonwealth University who analyzed data from 177,000 ex-military personnel diagnosed with dementia between 2009 and 2019 found that one in 10 also showed signs of severe liver cirrhosis – or scarring of the organ.
They suggested that many of these people may have been misdiagnosed and were instead suffering from hepatic encephalitis (HE) – or a brain disorder with symptoms similar to dementia.
The graph above shows how a healthy liver functions (left) and what happens when the liver stops working properly (right). In these cases, toxins build up in the brain, which can lead to dementia-like symptoms in a condition called hepatic encephalitis.
Unlike dementia, this can sometimes be reversed by medications, lifestyle changes or, in severe cases, surgery to transplant a healthy liver into the body.
Researchers point to two previous cases where dementia symptoms disappeared after liver treatment, with one woman saying her husband was now a ‘different person’.
If scientists’ estimates are correct, as many as 670,000 Americans may have been wrongly told they have dementia.
Liver cirrhosis is rarely noticed in the early stages because it is a ‘silent’ disease – and symptoms only become apparent when the damage is severe.
It can be caused by a variety of factors, including long-term alcohol abuse, persistent viral infections – such as hepatitis – and obesity leading to fatty liver disease.
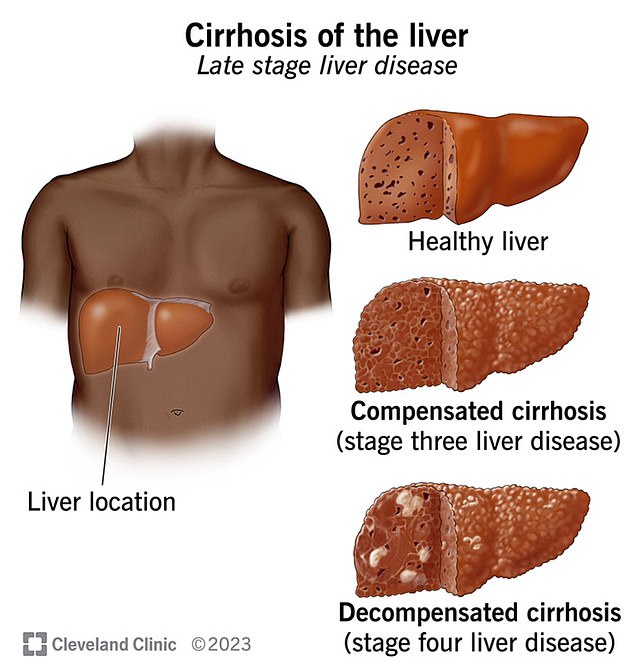
The above image shows the location of the liver and what a healthy liver looks like compared to a liver with cirrhosis or liver scarring
But the condition can lead to brain dysfunction, or HE, with patients experiencing confusion, mood swings and impulsive behavior – similar to dementia patients.
While it is not common for liver damage to be completely reversed to this extent, it can improve by treating the underlying cause, such as alcohol addiction or obesity.
In more extreme cases, patients may also be offered a full liver transplant.
However, the doctors noted that some cases of liver cirrhosis cause irreversible damage to the blood vessels in the brain, leading to symptoms of dementia.
They also said that in some cases it was possible that both dementia – which can also be caused by ‘lumps’ of amyloid beta in the brain – and liver cirrhosis could occur at the same time.
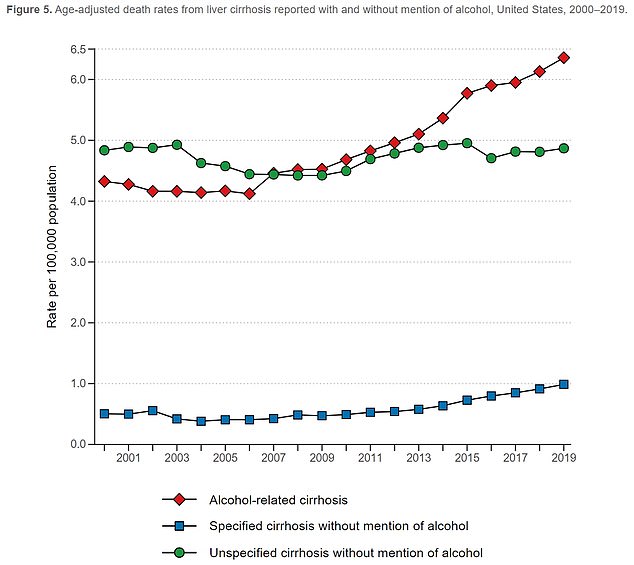
The graph above shows the age-adjusted death rates for liver cirrhosis per 100,000 people. These have increased in recent years as an increase in the number of dementia cases has also been reported
Doctors say it is difficult to distinguish patients with HE and dementia because there is no single blood test to separate the two.
But in many cases, patients are only screened for dementia – which is diagnosed using a series of cognitive tests – but not for liver cirrhosis.
Dr. Jasmohan Bajaj, a gastroenterologist at Virginia Commonwealth University who led the study, told DailyMail.com: ‘What we believe is that some people with dementia may have a reversible condition like HE.
‘Identifying and treating HE (carried out with commonly available medications) leads to improvements in mental functioning.
“So if this 10 percent has HE contributing to or masquerading as the brain dysfunction due to the dementia, then repairing the HE will help the mental dysfunction.”
He added: ‘We initially found this in two cases (revealed in 2022) where patients who had HE and had not been diagnosed as such but were being treated for dementia improved after receiving appropriate treatment for HE.’
Previous research has linked liver disease to a higher risk of dementia or Alzheimer’s disease.
But this paper is believed to be one of the first to suggest that such large numbers of dementia patients may have been misdiagnosed.
Previous research has also suggested that one in five patients with Alzheimer’s disease may have another condition, such as brain atrophy – where part of the brain loses neurons.
For the research, published in JAMA network openedresearchers looked at data from 177,000 veterans who were diagnosed with dementia between 2009 and 2019 but were not diagnosed with liver problems.
They then looked at each patient’s blood work to determine if they had signs of liver cirrhosis.
This checks levels of fibrinogen, a protein produced by the liver, and low levels of which indicate damage to the organ.
They found that up to 10 percent of patients had a score high enough – more than 2.67 – to indicate potentially serious liver disease.
Of these, half had a score above 3.25, which further indicates the risk.
The researchers said the test could not diagnose liver cirrhosis because it required more smears, but was an important indicator of the disease.
None of the patients in the study had been tested for liver cirrhosis.
The patients were on average 80 years old, mostly men, and had an average body mass index of 26, which put them in the overweight range.
Dr. Lauren Beste, deputy chief of general medicine at the VA Puget Sound Healthcare System, explained how the condition could be missed. STAT news: ‘It is not a condition that hurts. Patients do not come in asking to be screened for cirrhosis.
‘It’s easy to understand why it can be overlooked, but it’s such an important and life-saving diagnosis to make early.’
