Mayo Clinic doctor who made it his life’s mission to cure diabetes – after three of his children were diagnosed with a condition that will affect 1.5 BILLION people by 2050
A Mayo Clinic doctor is looking to cure diabetes within his lifetime after three children were diagnosed with the type 1 form of the condition.
Dr. Quinn Peterson, director of the Islet Engineering and Replacement Laboratory at the Mayo Clinic in Minnesota, was pursuing a career in developing chemotherapy drugs for cancer patients when his then-three-year-old daughter, Clarissa, was diagnosed with diabetes in 2010.
“That was a very important event in our family’s life,” he told DailyMail.com.
‘As a father, I felt a responsibility that if I could contribute in any way to alleviating the suffering of this disease, not only for my daughter, but for everyone who suffers from this disease, I had a responsibility to do so .’
Since Clarissa, who is now 17, was diagnosed, two of Dr.’s younger children have also been diagnosed. Peterson – daughter Sarah, 12, and son Seth, 8 – diagnosed.
Dr. Quinn Peterson (far left) shifted his focus to diabetes research after his eldest daughter, Clarissa (center), was diagnosed. He now leads a team at the Mayo Clinic working on treatments to ultimately cure the disease
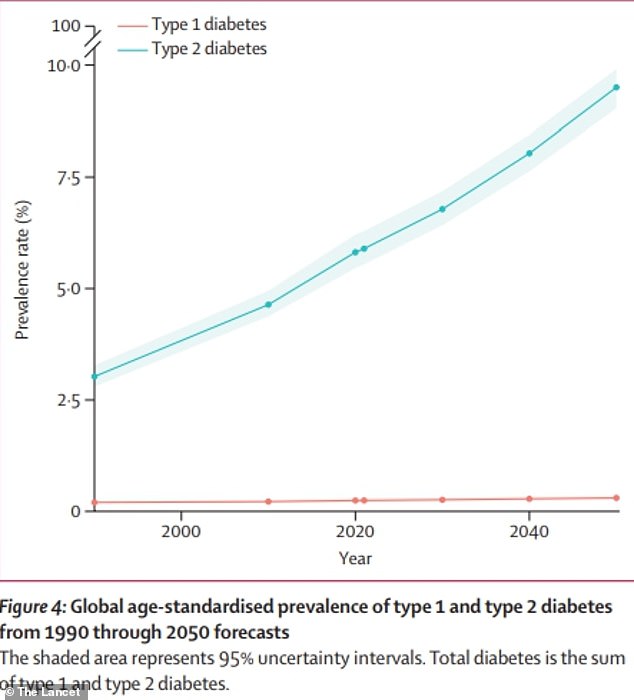
The above graph shows estimates for global diabetes cases. It is predicted that the number of people with the condition will more than double by the year 2050 compared to 2021
Dr. Peterson’s team is now developing a cell-based therapy that could replace the need for supplemental insulin – and it is already being tested.
Ultimately, he hopes that these types of treatments can completely cure diabetes, which is on the rise around the world.
‘It has been a very rewarding experience for me to be able to work on something that I have such a personal passion for. But that passion has only grown stronger since my children were diagnosed.”
Dr. Peterson noted that he has seen the challenges his children face while living with type 1 diabetes.
In addition to having to inject insulin every day, his children are also forced to feel like outsiders, such as missing birthday cake at parties and sitting outside during sports.
The family is also concerned about the complications the children will face, as the condition increases the risk of heart disease due to narrowed blood vessels and kidney and eye problems.
These problems mean that people with type 1 diabetes tend to die younger – with recent estimates suggesting that the decline in life expectancy could range from seven to 20 years.
Dr. Peterson’s team is working on a form of cell replacement therapy, in which diseased insulin-producing cells are replaced with healthy cells.

‘My children are incredibly brave. They are dealing with this disease with a lot of courage and a lot of confidence,” Dr. Peterson said of his children, three of whom have Type 1 diabetes.
Diabetes is a chronic condition in which the pancreas cannot produce enough beta cells, which make insulin. Insulin regulates blood sugar levels, also called glucose, which the body needs for energy.
When the body cannot produce enough insulin, too much blood sugar remains in the bloodstream. This can lead to heart disease, kidney disease, nerve damage and other lasting health problems.
According to the Centers for Disease Control and Prevention (CDC), approximately 38 million children in the US have diabetes, and one in five is undiagnosed.
In type 1 diabetes, an autoimmune reaction causes the body to stop producing insulin. This can be diagnosed at any age, and the CDC estimates that five to ten percent of Americans have it.
Type 2 diabetes, meanwhile, develops over many years and is usually diagnosed in adults. This happens when the body’s insulin cannot keep blood sugar levels at normal levels. Obesity is a major risk factor for this form, which affects more than 90 percent of diabetics.
Both type 1 and type 2 diabetes are on the rise, and the number of cases is expected to rise to 1.3 billion in the next three decades.
Experts estimate that the explosion in cases – more than double the current 529 million – will be driven largely by the world’s ever-expanding waistline.
From a study published last year in the Journal of the American Heart AssociationFor example, research has found that obesity is linked to 30 to 53 percent of new diabetes cases in the U.S. each year.
The CDC estimates that four in 10 Americans are obese, and that rate is rising. For example, between March 2020 and March 2021, the number increased by 3 percent.
Dietary factors may play a role, as the American diet is high in sugar and processed foods – known risks for the condition.
Dr. Peterson and his team are working on cell replacement therapy for type 1 diabetics, in which new, healthy cells are placed in the body to replace diseased or damaged cells.
In this case, immature stem cells would be transformed into cells that function similarly to beta cells. It can also be made into cells that mimic the function of alpha cells, which produce a hormone called glycogen that functions similarly to glucose and increases blood sugar levels.
These cells are normally found in an area of the pancreas called the islet.
‘These three cell types work together as a community. They communicate with each other. They signal each other to work together to regulate blood sugar levels,” Dr. Peterson said.
“This would be a cell product that we could transplant into these individuals, which would then allow these individuals to produce their own insulin instead of having to receive daily insulin injections.”
‘The cells we generate are like a living drug that would be able to sense the amount of glucose in the environment and secrete the right amount of insulin for these patients.’
This would also replace the need to monitor blood sugar levels, which Dr. Peterson does for his children several times a day, from the time they wake up until they go to bed.
Although the team is primarily evaluating treatment in patients with type 1 diabetes, Dr. Peterson said there could also be potential benefit in people with type 2 diabetes.
Patients could expect this through a minor operation where the cells would be implanted just beneath the skin’s surface.
Dr. Peterson estimates that the cells can survive for about five years.
“For individuals who have this disease, we are optimistic that as we continue clinical trials, we will see significant improvements in the standard of care for patients,” he said.
However, he warns that it may be several years before cell therapy is used in human clinical trials, and even longer before it becomes the standard of care.
Still, he remains optimistic about the potential.
‘This gives me a lot of hope. I see every day the struggle of living with this disease,” said Dr. Peterson.
‘My children are incredibly brave. They deal with this disease with great courage and confidence.
“But there are quiet moments where they share with me and my wife the struggle they face with this disease, the difficulty it is for them on an emotional level, on a personal level, on a physical level.”
‘For me, the idea of developing a cell replacement therapy offers a lot of hope, not only for my children, but for all patients who struggle with this, that their suffering can be alleviated.’
‘They can have hope for a future where type 1 diabetes is not the challenge it is today, and that they can live a normal life without the stress that this disease brings.’
