Cushla Rabbitt lost her daughter to darkness so she’s building a place of light
OOn the outskirts of a regional town in Queensland, Cushla Rabbitt stands in an old warehouse under renovation. Sunlight streams through the skylights as tears swell around her eyes. It’s a new beginning.
Three years have passed since her 30-year-old daughter, Heather Stuart, committed suicide. The year before her death, one of Rabbitt’s cousins died by suicide. The following year, so did another.
“I had to ignore my emotions, sadness and desire to break down in order to remain logical, because no one else would do it,” Rabbitt says. She couldn’t stop and grieve; she had to organize a funeral.
But she was broke. She couldn’t afford the funeral director in town, so she called around until she found one for half the price.
There was no hearse or coffin. Her daughter’s body was taken from a Brisbane mortuary, placed on a trolley and loaded into the back of a van. When it arrived in Warwick, a town two hours’ drive west, her family carried the body inside and laid it on a mattress in Rabbitt’s bedroom.
The room became tapu – sacred, in her Māori culture. Under oppressive summer heat, her body lay on a block of ice for three days. Family came and went, observing strict Māori customs. On the last day, Rabbitt lay on the floor next to the mattress and held her daughter’s hand. “We wrapped her like a burrito in all the sheets and that was it,” Rabbitt says. She said goodbye for the last time and cried.
Heather’s suicide rippled through her family. One self-harmed, others contemplated or attempted suicide. “And I guess you can count me too,” Rabbitt says. “I’ve had my own journeys on that.”

In regional Queensland there are few places to go for support. It was difficult to find mental health care appropriate for surviving family members. The services they did have access to felt bureaucratic and it could take months to get an appointment.
“The mental health system here may be quite broken – people are finding it very difficult to navigate. They feel like it’s a systematic ticking and ticking,” says Maritta Hutley, chair of a local suicide prevention network that opened on the Darling Downs last year. The suicide rate for the region is almost double the national average. And the further west you go, the worse these numbers get.
Five weeks after Heather’s suicide, Rabbitt was back at work, but it took her much longer to come to terms with her daughter’s death. After two years she went to the Warwick Big Anxiety Festival – a University of New South Wales-led initiative exploring community and cultural responses to trauma. There she met other women with similar experiences. “It unleashed something in me,” she says.
Composite risk factors
Dr. Samara McPhedran, an honorary associate professor at the University of Queensland, says a family member committing suicide can increase the risk of others doing the same. When mental health care is difficult to access, these risks can increase.
Queensland also has a higher proportion of Aboriginal and Torres Strait Islander people compared to other states. The suicide rate among indigenous people is double that of non-indigenous people.

“We feel that if we can just treat mental illness, we can prevent suicide,” McPhedran says. “But we have taken this approach for many years and unfortunately we see suicide rates rising or remaining stable, but rarely falling in regional areas.
“I’m not for a moment saying that mental health care isn’t important. But these services do not always understand the needs of individual communities because they are branches of much larger services.”
Social connection, support, and participation are all well-documented components of suicide prevention. But across Australia, social cohesion is at its lowest level in sixteen years, while participation in social, community and civic groups is also declining.
In his latest mental health guidelines The World Health Organization says more attention needs to be paid to community-based care services to tackle mental health crises.
Susi Tegen, the CEO of the National Rural Health Alliance, says grassroots approaches to tackling mental health can play a supportive role in addition to the government’s long-term policy.
“Community projects like Big Anxiety are great,” she says. “But family, friends – they are not psychologists. Ultimately, we need more doctors.”
A trauma cycle
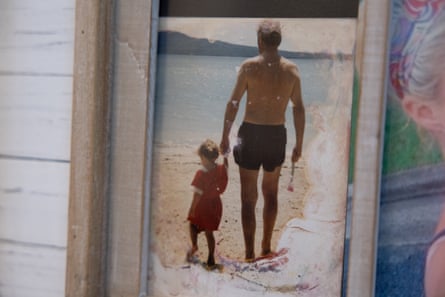
Every morning, Rabbitt has an imaginary conversation with a photo of Heather on her bedside table.
She talks to two-year-old Heather, who wandered along an Auckland beach holding her grandfather’s hand. To the imaginative child, determined to survive her miserable circumstances in New Zealand, who improvised a costume one Halloween with a few twigs and an old broomstick. To the woman who acted with unwavering selflessness towards others, no matter the cost to herself.
The last time Rabbitt saw Heather alive was on her thirtieth birthday. They ate fish and chips and took family photos on a cloudless day on the coast. For a moment it felt like they were a functioning family. “It was peaceful and beautiful,” she says. But then Heather disappeared again.
Since Heather was a teenager, she has drifted between the city and regional towns while struggling with substance abuse and worsening mental illness. She had a criminal record and no prospects of finding work. Because she was a New Zealand citizen – Rabbitt moved to Australia with her five children in the mid-2000s – she was not entitled to full government support. “And I would cut her off,” Rabbitt says. “She had nowhere to go.”
Eight months after her birthday, a week after she was released from prison, Heather was found dead in a public toilet in a town on the outskirts of Brisbane. It was Australia Day.
“I think she was the only other person on this planet who really understood me because she saw me going through things from the beginning,” Rabbitt says.
Rabbitt arrived in Australia with a suitcase and the opportunity for a well-paying job. After four months, she had enough money to send Heather and her four other children along.
It took another five years before they were safely established. “I lifted my children out of poverty, but it came at a huge cost,” she says. “It was a self-fulfilling prophecy with Heather. We were repeating our cycle, our cycle of trauma.”
Each week, Rabbitt meets with a handful of women she met on the Big Anxiety Project. Many have lost children or other family members to suicide. They’ve all been there victims of some form of abuse, including domestic violence.
McPhedran says there is increasing recognition that exposure to domestic violence is a common factor among young people who die by suicide. “That could be when you see a parent being abused by another parent, stepparent or adult,” she says. “That’s often associated with leaving home at a young age – which brings with it other risks of suicide, such as substance abuse, homelessness and criminal activity.”

Inside the warehouse in Warwick, Rabbitt imagines colorful murals painted on the walls.
The space will open to the community in a few weeks. Most of all, it means that her women’s group has a dedicated space to relax. But over time they hope it will become a home to a range of community and support groups. in addition to the clinical mental health care is already available in the city.
Heather had no refuge or family to turn to, nor access to the right support or services. Rabbitt hopes this space can change that for others.
“If we don’t give our children the tools to break the cycle of trauma and abuse, we are repeating history,” she says. “All I have to do is start.”
